Journal of Gynecological Research and Obstetrics
Hematocolpos on imperforated hymen and acute urinary retention A rare disease About seven observations and literature reviews
M Lahfaoui*, H Benhaddou and F Ettaybi
Cite this as
Lahfaoui M, Benhaddou H, Ettaybi F (2020) Hematocolpos on imperforated hymen and acute urinary retention A rare disease About seven observations and literature reviews. J Gynecol Res Obstet 6(2): 014-018. DOI: 10.17352/jgro.000079Hymenal imperforation is a fairly rare malformation, and severe when ignored. Based on the literature data on this malformation, a retrospective study was conducted on 7 cases of haematocolpos on imperforated hymen, collected to the uro-visceral pediatric surgery departments, Children’s Hospital, Oujda-Rabat (MOROCCO), over a period from January 2011 to January 2019. It appears from this work that this anomaly is the prerogative of patients in the peripubertal period. The clinical signs is dominated by abdominal and pelvic pain. The existence of an abdominal-pelvic tumefaction in all our patients and by urinary complications such as acute urine retention in 3 of our 7 cases. The diagnosis is mainly clinical and is oriented by ultrasound. Hymene imperforation remains the most frequent etiology, it is found in our 7 patients, The surgical treatment is simple carried out on an incision of the obturating diaphragm, and a drainage of the collection.
Introduction
Hymenal imperforation is a relatively rare but the most common congenital malformation of the female genital tract (1). It is often isolated but sometimes associated with malformations of the urogenital tract (2).
Painful cryptomenorrhea by parapubertal hymenorrhoea is the most classic telltale picture (3). Non-gynecologic symptoms sometimes mislead the diagnosis.
Hymenal imperforation is easily diagnosed by inspection of the external genitalia. Ultrasonography has simplified the analysis of this rare pathology, and is the best method for early diagnosis thanks to in utero ultrasound.
Hymenotomy is the treatment of hematocolpos by hymenal imperforation. For hematocolpos revealing malformations, the treatment of the causal malformation is more complex.
Early diagnosis and treatment of hymeal imperforation is important in order to improve the prognosis and avoid any tubal sequelae.
In our work, we report a series of seven Hymenal imperforations.
Case reports
a) Case 1
13 year old patient, admitted for management of an acute abdominal picture with the notion of cyclic pain for five months. She has not had her menarche, but has developed sexual characteristics (breasts at S4 and pubic hair at P5). Examination showed a slight bulging of the hymen and the recto-vaginal septum. Ultrasound showed hematocolpos. Surgical incision of the Y-shaped hymen allowed 600 milliliters of black blood to be drained. The evolution is favourable at the follow-up examination of the patient after three weeks. A forensic certificate of medical loss of virginity is given to the family.
b) Case 2
15-year-old patient admitted to pediatric emergency department for cyclical pelvic pain for 9 months with exacerbation of pain for 7 days without urinary signs with pelvic mass of 12cm, at ultrasound the uterus is in place measuring 9.3/5.1 cm regular with endocavitary fluid retention finely echogenic communicating via the cervical os with hematosalpinx. Treated through an O incision, it consists of excising a small central collar of the hymen through which a Foley catheter is inserted. The balloon of the catheter is inflated to 10 cm3 and the catheter is removed after 2 weeks. Drain 1200cc of black blood. The evolution is satisfactory. A medical-legal certificate of medical loss of virginity is given to the family.
c) Case 3
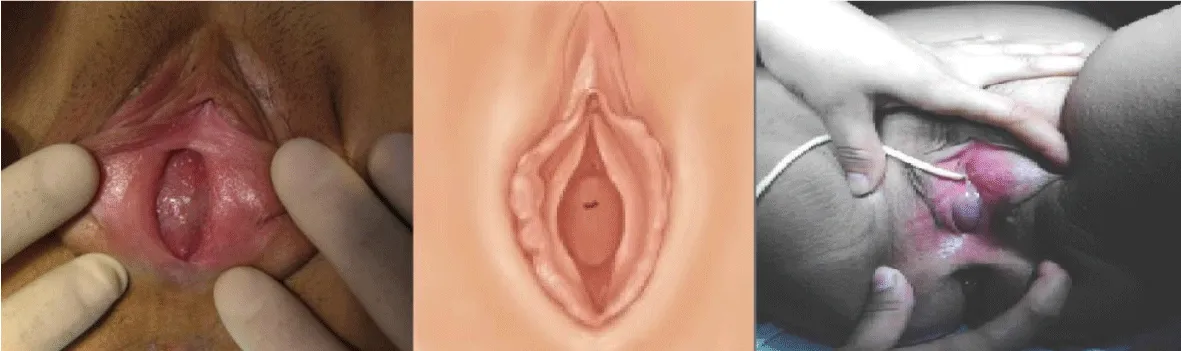
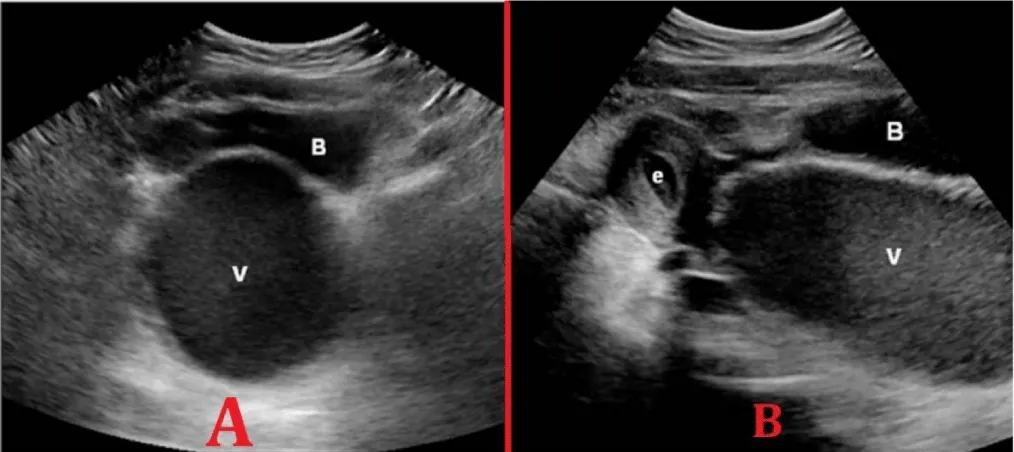
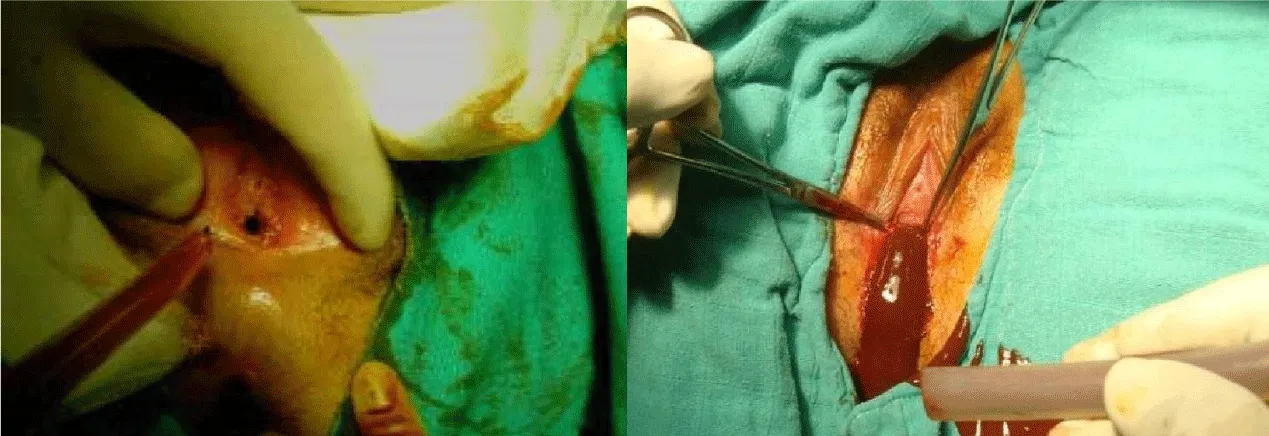
A 14-year-old patient admitted to the pediatric emergency department with pelvic pain 9 days prior to admission with complicated acute urinary retention since 18:00 on abdominal and pelvic examination, there was a 12-cm mobile renal pelvic mass with a bladder globe (Figure 1), good external genital development and secondary sexual characteristics with a bluish, bulging, imperforate hymen (Figure 2). An emergency ultrasound scan was performed to show a hematocolpos with right hematosalpinx (Figure 3). a Y-shaped incision of the hymen with drainage of 500 cc of blackish blood plicature of the flaps with vicryl 6(0) to the wall placement of a 16ch bladder catheter in the vagina for 7 days .evolution without stenosis .the orifice was dilated once a week for 1 month then once every two weeks then once every three months. A medical-legal certificate of medical loss of virginity is given to the family.
d) Case 4
Patient, 13 years and 6 months old, admitted for management of an acute abdominal picture with the notion of cyclic pain for four months. She has not had her menarche, but has developed sexual characteristics, with a first-degree (sister) family history of hematocolpos.
Examination showed a slight bulging of the hymen and the recto-vaginal septum. Ultrasound revealed hematocolpos. Surgical incision of the Y-shaped hymen allowed 500 milliliters of blackish blood to be drained. Dilatation was performed every 10 days after discharge, once a week, then once a fortnight, then once a month. The evolution is favourable at the time of the patient’s follow-up examination after three months. A medical-legal certificate of loss of virginity is given to the family.
e) Case 5
A 14-year-old patient admitted to the pediatric emergency department for pelvic pain dating back 2 days before her complicated admission with acute urinary retention for 12 hours on examination of the abdomen showed an oval-shaped suprapubic swelling, with a large upper extremity, regular contours, fluctuating or renal consistency, sensitive, matt to percussion, and plunging down behind the pubic symphysis. Inspection of the vulva allows recognition of imperforation by showing a bluish translucent membrane protruding between the labia minora with good development of the external genitalia and secondary sexual characteristics. An ultrasound scan performed urgently to show a haematocolpos. A Y incision of the hymen with drainage of 600 cc of blackish blood plicature of the flaps with vicryl 7(0) to the wall placement of a bladder probe 18ch in the vagina for 7 days .an evolution without stenosis .the orifice was dilated once a week for 1 month then once every two weeks then one every three months. A medical-legal certificate of medical loss of virginity is given to the family.
f) Case 6
Thirteen-year-old patient admitted to the pediatric emergency department for pelvic pain dating back 4 days before her admission with complicated acute urine retention since 12 hours. On abdominal and pelvic examination, there was a 10 cm mobile renal pelvic mass with a bladder globe, a good development of the external genitalia and secondary sexual characteristics with a bluish imperforated and bulging hymen, and an ultrasound scan performed urgently to show a hematocolpos. An O-shaped incision of the hymen with drainage of 400 cc of blackish blood and placement of a 16ch bladder catheter in the vagina for 15 days, with no stenosis. A forensic certificate of medical loss of virginity is given to the family.
g) Case 7
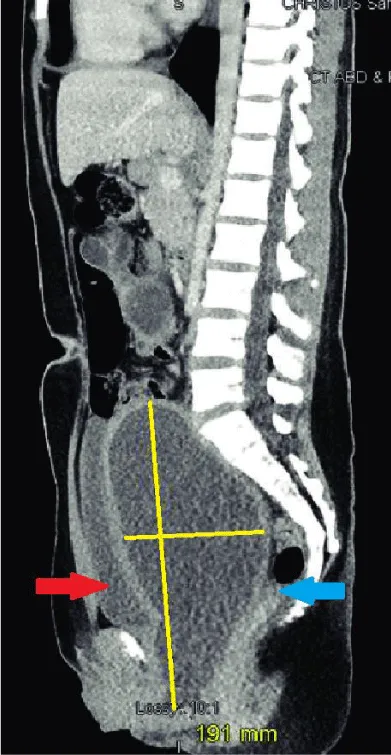
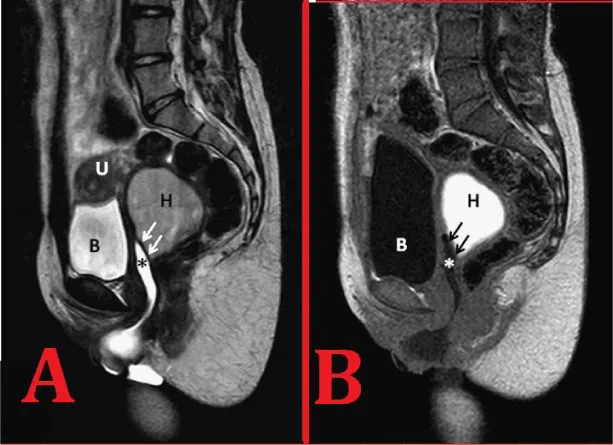
14-year-old patient admitted to pediatric emergency department for cyclical pelvic pain for 5 months with exacerbation of pain for 4 days without urinary signs with pelvic mass of
13cm, at ultrasound the uterus is in place measuring 9.7/5.6 cm regular with endocavitary fluid retention finely echogenic communicating via the cervical os, retro bladder collection finely echogenic with 9.5/5.1 cm thickened wall. O-shaped incision. 500cc drainage of blackish blood (Figures 4-6), passage of a catheter into the vagina. This catheter is then removed after 2 weeks. The evolution was satisfactory. A forensic certificate of medical loss of virginity is given to the family.
The evolution of our patients was judged on the functional and morphological state, a complete cure was obtained in our seven patients without relapse.
Results and discussion
The hymen is a remnant of the mesodermal leaflet that normally perforates during the later stages of embryonic development [4]. Hymenal imperforation is a rare event estimated at 1 in 2000 female births, but the most common congenital malformation of the female genital tract [1,4,5]. The incidence reported in the literature is widely variable, depending on whether it is assessed globally, according to age or according to the type of anatomical lesion [6]. In typical cases, the age of discovery of hematocolpos is between 12 and 15 years (the age of menarche) [7,8]. In our series of 7 hematocolpos cases, the age of our patients varies between 13 and 15 years (the pubertal period). The majority of cases reported in the literature are sporadic, however, a few familial cases have been described suggesting a probable genetic predisposition [5,9]. Only one patient among the cases we have presented has a family history of hymenal imperforation.
The diagnosis of hymenal imperforation is possible in utero when a hydrometrocolpos is found on ultrasound [10,11]. The in utero diagnosis also has the added advantage of looking for associated renal malformations. This diagnosis can be made by systematic screening at birth but also in front of a hydrometrocolpos of the newborn female baby [12]. Most often, this malformation is discovered at puberty. The diagnosis should be suspected in a girl with primary amenorrhea with normally developed secondary sexual characteristics. Patients usually consult for recurrent pelvic pain secondary to blood accumulation in the vagina or hematocolpos [13]. The cyclical nature of the painful attacks may be missed because of the usual irregularity of the menstrual cycle in the peripubertal period [14]. Pain may be misleading, pseudoppendicular and may induce ‘overdoing’ procedures on suspicion of acute appendicitis [15]. Haematocolpos can compress the urethra and cause dysuria, complete bladder retention and even bilateral ureterohydronephrosis [13,16-19,20]. Einsenberg [21] reported 7 cases of bladder retention in a series of 44 haematocoplos observations [13,16-19,20]. Constipation is due to the same compressive mechanism [22]. In our series all the patients were not yet menarche. All patients have good development of external genitalia and secondary sexual characteristics.
Five patients presented with cyclic pain before. Abdominal-pelvic pain dominated the functional picture, it was observed in all cases. Three of our patients reported urinary signs of acute urinary retention. None of our patients showed signs of vascular, nervous or digestive compression. Blood is retained first in the vagina, then in the uterus (hematometry) and eventually in the fallopian tubes. Its volume varies from one patient to another and can even reach 3 litres [9]. Retrograde menstrual flow can alter the fallopian tubes or lead to endometriosis lesions that can impair fertility later [23]. However, this is rare if the diagnosis is made early and fertility is usually maintained [24-26]. Clinical diagnosis of this malformation is usually easy. Examination of the abdomen reveals an oval-shaped suprapubic swelling, with a large upper end, regular contours, fluctuating or renal consistency, sensitive, dull to percussion, and plunging down behind the pubic symphysis. Inspection of the vulva allows imperforation to be recognized by showing a bluish translucent membrane protruding between the labia minora. The digital rectal examination reveals a median, anterior swelling of fluid consistency, renal, extending with the abdominal mass and descending close to the anal sphincter.
In our series The genital examination shows the existence of a hymen imperforation with a bulging imperforated hymen in the 7 patients, palpation was able to objectify the existence of a mass in all the patients.
In case of diagnostic uncertainty, ultrasonography may be useful in showing the hematocolpos as a median, retrovesical fluid tone image containing some heterogeneous echoes. It also makes it possible to assess the impact upstream of menstrual retention by looking for haematometry, haematosalpinx and intraabdominal effusion [27]. MRI is used to explore pelvic masses and utero-vaginal malformations. These advantages are especially valid in cases where ultrasound diagnosis is difficult. Laparoscopy makes it possible to establish a precise assessment of the lesions upstream and to treat possible endometriosis and perianxillary adhesions secondary to chronic inflammation [10]. It is especially indicated in the case of significant haematocolpos which gives rise to fears of upstream repercussions [10,11,12,28].
In our study, abdominopelvic ultrasound was performed in all patients; the ultrasound was complementary to the clinically confirmed diagnosis. It revealed uterine and intravaginal fluid collection in favour of haematocolpos.
The objectives of this treatment are surgical:
➢ To restore the permeability of the genital tract.
➢ Ensure normal sexual function.
➢ Attempt to preserve future fertility.
It must be undertaken in all cases, never rely on spontaneous regression of retentions. Abstention, even in mild forms, could lead to the development of genital and urinary tract infections, which are more frequently encountered in late-onset forms. In many cases, treatment is limited to simple drainage of the retained pouch. Total circumferential excision of the hymen may lead to sclerosis and orifice dyspareunia [28,29]. It should therefore be avoided. Hymenotomy must allow normal menstrual flow, trying to respect the virginity of these young patients as much as possible, especially in our social context, and to ensure a normal sexual life later on by avoiding restenosis. To do this, it is necessary to respect the orifices of the Bartholin glands at 5 o’clock and 7 o’clock and to make an incision at 11 o’clock in the gynaecological position in order to free the lower bank of the urinary meatus and to ensure meatohymenal dissociation. Several surgical techniques are proposed in the literature. Salvat [30], recommends the technique of radial star-shaped hymeal incisions, which is simple but does not guarantee virginity. Another technique has been described by Ali, et al. [31]. It consists of excising a small central collar of the hymen through which a Foley probe is inserted. The balloon of the catheter is inflated to 10 cm3 and the catheter is then removed after 2 weeks. We found this technique interesting because it is simple, less invasive than other methods and preserves the normal architecture of the hymen. The only disadvantage of this technique is the secondary discomfort of wearing the catheter for 2 weeks. This technique is practiced in 3 of our patients. The results of this technique are rather encouraging: only 2 patients out of 65 have presented secondary hymenal stenosis in the Acar series [31]. In all cases, a postoperative clinical check-up must be systematic to verify the absence of secondary stenosis. This said, the best treatment remains preventive, based on early diagnosis of the malformation and on surgery undertaken after development of the genital organs but before the appearance of haematocolpos [32].
In our series, the 7 patients with hematocolpos on a hymeneal imperforation benefited from a Y and O incision of the hymen, evacuation of the hematic collection, and drainage by a catheter left in place for 7-10 days for the Y incision, and 15 days for the O incision. All patients were put under a bi-antibiotherapy, local care several times a day, and dilatation sessions according to the evolution.
The evolution in the 7 cases of hymeneal imperforation was satisfactory without postoperative stenosis.
Conclusion
Hymenal imperforations are a group of genital malformations. It is an often benign condition, with a favourable evolution, if diagnosed and treated early. On the other hand, its lack of knowledge exposes it to serious complications, threatening its vital prognosis and seriously compromising its obstetrical future. Ultrasonography remains the examination of choice to confirm the diagnosis, and makes it possible to identify possible upstream repercussions and possible associated urogenital anomalies. Systematic screening at birth and early treatment are the best guarantee of preventing complications of this pathology. We observed 7 hematocolpos cases secondary to a lack of knowledge of an imperforate hymen. As delivery rooms in our country cannot be accompanied by paediatricians, the training of midwives, insisting on the systematic examination of newborns, will make it possible to recognize malformations at birth, including imperforation of the hymen. This would avoid emergency situations that sometimes lead to inappropriate treatment. The treatment is exclusively surgical and the routes of access are different. Most often, it remains remarkably simple and leads to a definitive cure.
- Messina M, Severi FM, Bocchi C, Ferrucci E, Di Maggio G, et al. (2004) Voluminous prénatal masse: a case f congénital hydrometrocolpos. J Matern Fetal Neonatal Med 15: 135-137. Link: https://bit.ly/3c2Y4k3
- Yanza MC, Sepou A, Nguembi E, Ngbale R, Gaunefet C, et al. (2003) Hymen imperforé, diagnostic négligé à la naissance, urgence chirurgicale à l’adolescence. Schweiz Med Forum 44: 1063-1065.
- Salvat J, Slamani L (1998) Hématocolpos. J Gynécol Obstet Biol Reprod (Paris) 27: 396-402. Link: https://bit.ly/2yr7Cqr
- Heger AH, Ticson L, Guerra L, Lister J, Zaragoza T, et al. (2002) Appearance of the genitalia in girls selected for nonabuse: review of hymenal morphology and nonspecific findings. J Pediatr Adolesc Gynecol 15: 27-35. Link: https://bit.ly/2YuAZTy
- Walsh B, Shih R (2006) An unusual case of urinary retention in a competitive gymnast. J Emerg Med 31: 279-281. Link: https://bit.ly/3fjS8Fh
- Battran VC (1983) Mullerian anomalies and their management. Fertil steril 40: 159-163. Link: https://bit.ly/2z6AO6k
- Hall DJ (1999) An usual case of urinary retention due toimperforate hymen. J Accid Emerg Med 16: 232-233. Link: https://bit.ly/3c1nxKF
- Letts M, Haasbeek J (1990) Hematocolpos as a case of back pain in premenarchal adolescents. J Pediatr Orthop 10: 731-732. Link: https://bit.ly/2Yv0unB
- Sakalkale R, Samarakkody U (2005) Familial occurrence of imperforate hymen. J Pediatr Adolesc Gynecol 18: 427-429. Link: https://bit.ly/35uFS0g
- Salvat J, Slamani L (1998) Hématocolpos. J Gynécol Obstet Biol Reprod 27: 396-402. Link: https://bit.ly/3b0jsVR
- Winderl LM, Silverman PK (1995) Prenatal diagnosis of congenital imperforate hymen. Obstet Gynecolb 85: 857-860. Link: https://bit.ly/3ce3hFG
- Rochet Y (1986) les principales malformations génitales: Aspects thérapeutiques. Rev Fr Gyn Obstet 81: 315-317.
- Adali E, Kurdoglu M, Yildizhan R, Kolusari A (2009) An overlooked cause of acute urinary retention in an adolescent girl: a case report. Arch Gynecol Obstet 279: 701-703. Link: https://bit.ly/2xwmjIq
- Paniel BJ, Truc JB, Beuzit JM, Pelissier C (1987) Diagnostic des malformations congénitales de la vulve et du vagin. Ann Pédiatr 34: 11-25. Link: https://bit.ly/2z9gdxY
- Emans SJ, Laufer MR, Goldstein DP (2004) Dysmenorrhea, pelvic pain, and the premenstrual syndrome. In: Emans SJ, Laufer MR, Goldstein DP, eds. Pediatric and Adolescent Gynecology 5th ed. Philadelphia : Lippincott-Raven 376-384.
- Loscalzo IL, Catapano M, Loscalzo J, Sama A (1995) Imperforate hymen with bilateral hydronephrosis: an unusual emergency department diagnosis. J Emerg Med 13: 337-339. Link: https://bit.ly/3deX9gA
- Yu TJ, Lin MC (1993) Acute urinary retention in two patients with imperforate hymen. Scand J Urol Nephrol 27: 43-44. Link: https://bit.ly/2Sw71uI
- Dane C, Dane B, Erginbas M, Cetin A (2007) Imperforate hymen-a rare cause of abdominal pain: two cases and review of the literature. J Pediatr Adolesc Gynecol 20: 245-247. Link: https://bit.ly/35ybQJg
- Wort SJ, Heman-Ackah C, Davies A (1995) Acute urinary retention in the young female. Br J Urol 13: 337-339.
- Chang JW, Yang LY, Wang HH, Wang JK, Tiu CM (2007) Acute urinary retention as the presentation of imperforate hymen. J Chin Med Assoc 70: 559-561. Link: https://bit.ly/2ytePX0
- Einsenberg E, Faber M, Mitchell GW Jr, Turksoy RN, Rule AH (1982) Complete duplication of the uterus and cervix with unilateraly imperforate vagina. Obst Gynecol 60: 259-262. Link: https://bit.ly/2YuD024
- Wang W, Chen MH, Yang W, Hwang DL (2004) Imperforate hymen presenting with chronic constipation and lumbago: report of one case. Acta Paediatr Taiwan 45: 340-342. Link: https://bit.ly/3fidsex
- Olive DL, Henderson DY (1987) Endometriosis and mullerian anomalies. Obstet Gynecol 69: 412-415. Link: https://bit.ly/3c5h2Xe
- Rock JA, Zacur HA, Dlugi AM, Jones HW Jr, TeLinde RW (1982) Pregnancy success following surgical correction of imperforate hymen and complete transverse vaginal septum. Obstet Gynecol 59: 448-451. Link: https://bit.ly/35vQTPa
- Liang CC, Chang SD, Soong YK (2003) Long-term followup of women who underwent surgical correction for imperforate hymen. Arch Gynecol Obstet 269: 5-8. Link: https://bit.ly/2xxz0mh
- Joki-Erkkilä MM, Heinonen PK (2003) Presenting and longterm clinical implications and fecundity in females with obstructing vaginal malformations. J Pediatr Adolesc Gynecol 16: 307-312. Link: https://bit.ly/2YvwMPn
- Robberecht E, Smets A, Wincker MV, Delens F (1996) Radiological case of the month hematocolpos due to imperforate hymen. Arch Pediatr Adolesc Med 150: 993-994. Link: https://bit.ly/3aVb2z6
- Chelli D, Kehila M, Sfar E, Zouaoui B, Chelli H, et al. (2008) Imperforation hyménéale : peut-on la traiter en préservant la virginité. Santé 18: 83-87. Link: https://bit.ly/2WmoIhe
- Salvat J, Slamani L (1998) Hématocolpos. J Gynécol Obstet Biol Reprod (Paris) 27: 396-402. Link: https://bit.ly/2yr7Cqr
- Ali A, Cetin C, Nedim C, Kazim G, Cemalettin A (2003) Treatment of imperforate hymen by application of Foley catheter. Eur J Obstet Gynecol Reprod Biol 106: 72-75. Link: https://bit.ly/3ce5ile
- Acar A, Balci O, Karatayli R, Capar M, Colakoglu MC (2007) The treatment of 65 women with imperforate hymen by a central incision and application of Foley catheter. BJOG 114: 1376-1379. Link: https://bit.ly/3b0zrTX
- Ramsiss H, Harrak H, Amrani S, Elyoussfi M, Bargach S (2015) Hematocolpos Sur Imperforation Hymeneale a Propos De 3 Cas. Global Journals Inc. Link: https://bit.ly/2xBVq64
Article Alerts
Subscribe to our articles alerts and stay tuned.
 This work is licensed under a Creative Commons Attribution 4.0 International License.
This work is licensed under a Creative Commons Attribution 4.0 International License.


 Save to Mendeley
Save to Mendeley
