Archives of Clinical Gastroenterology
A Rare Benign Pancreatic Lesion Mimicking Malignancy- Eosinophilic Pancreatitis
Kurşat Rahmi Serin1, Muharrem Oner1, Nadir Adnan Hacım1* and Ali Emre2
2VKV American Hospital Nişantaşı, Istanbul, Turkey
Cite this as
Serin KR, Oner M, Hacım NA, Emre A (2018) A Rare Benign Pancreatic Lesion Mimicking Malignancy- Eosinophilic Pancreatitis. Arch Clin Gastroenterol 4(2): 020-022. DOI: 10.17352/2455-2283.000052Background: Eosinophilic infiltration of the pancreas is usually associated with generalized diseases like "sclerosing pancreatitis", "eosinophylic gastroenteritis" and "systemic mastocytosis". Most patients have systemic findings such as eosinophilia, elevated IgE levels and gastrointestinal tract infiltration Isolated eosinophilic infiltration of the pancreas is much less common and is usually found in the histological evaluation of pancreatic specimens resected with the misdiagnosis of pancreatic cancer.
Methods: Here in we report a rare benign pancreatic tumor that was operated on with the misdiagnosis of malignancy.
Results: A 47-year-old woman underwent laparotomy with the diagnosis of cholestasis and suspected stone image in the common bile duct. No stone was found in the biliary tract; however, a pancreatic head mass was discovered. It was considered unresectable. Cholecystectomy and T-tube drainage was performed. The operative biopsy was non-diagnostic and the patient was referred to our clinic. Radiologic findings revealed a resectable pancreatic head mass. A standard pancreatoduodenectomy was performed. The postoperative period was uneventful. Tissue diagnosis was "eosinophilic pancreatitis", without stomach, duodenum, and proximal jejunum involvement. No inflammation was detected on postoperative colonoscopy.
Discussion: Rare inflammatory pancreatic diseases such as eosinophilic pancreatitis mimics malignancy. If a definitive diagnosis can be achieved before operative decision, the disease can be treated nonsurgically.
Introduction
Eosinophilic infiltration of the pancreas is an uncommon finding. Most patients with eosinophilic infiltration of the pancreas have systemic manifestations such as eosinophilic infiltration in other parts of the gastrointestinal tract.
Isolated eosinophilic infiltration of the pancreas is a rare entity consisting of less than 1% of resected pancreatic specimens [1]. Herein we report a case of eosinophilic pancreatitis diagnosed after resection while it was previously thought to be malignant mass in the head of the pancreas.
Case Report
A 47-year-old woman was admitted to a state hospital with the complaints of jaundice, high fever and pain in the right upper abdomen. Abdominal ultrasonography revealed a dilated common bile duct and hydropic gall bladder without stone. However, a suspicious image of a calculus in the distal part of the common bile duct was encountered in the magnetic resonance cholangiopancreatography (MRCP). As endoscopic retrograde cholangiopancreatography (ERCP) was not available, an operative intervention was undertaken.
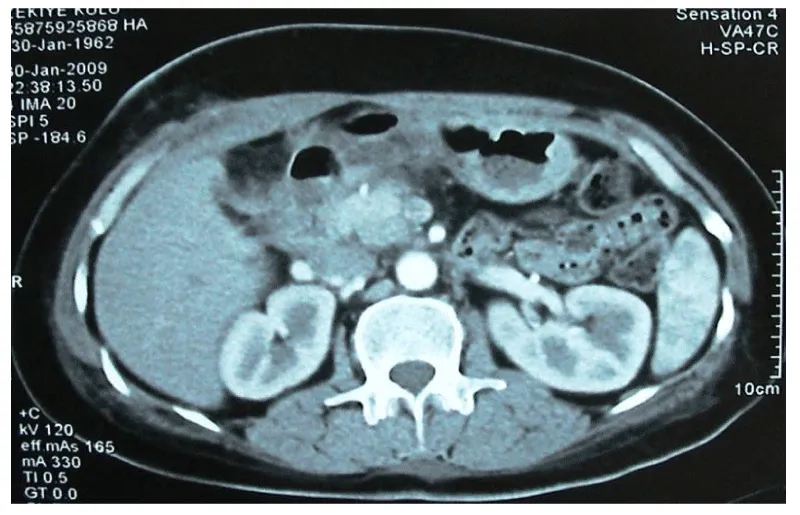
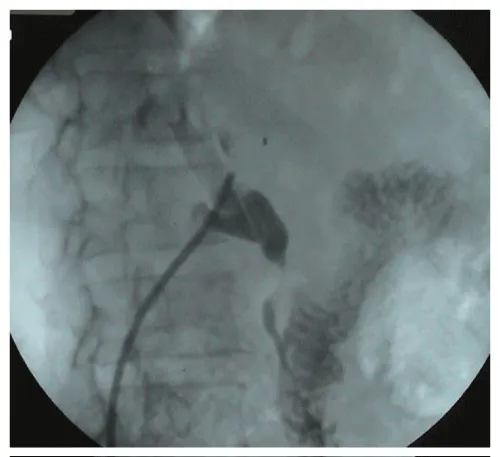
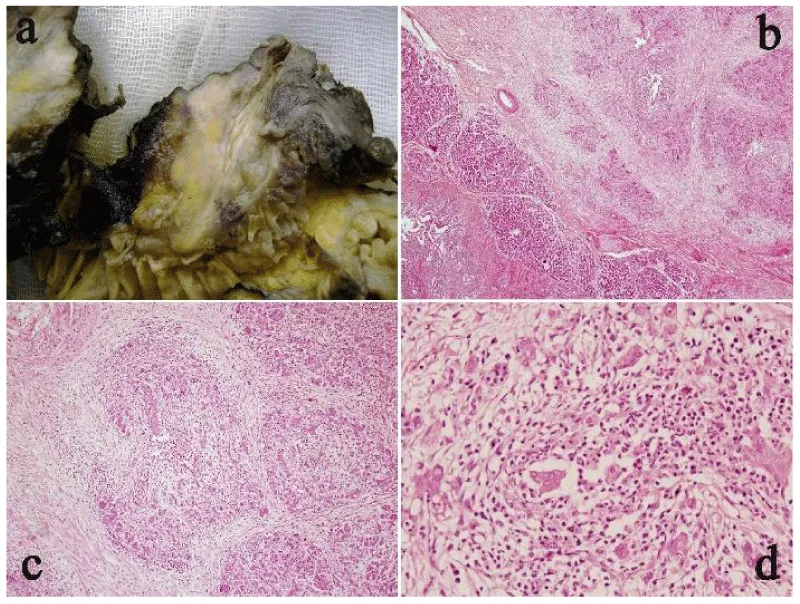
During the surgery, a fibrotic-hard and unresectable mass (The appearance was thought to be a vascular invasion) was palpated at the head of the pancreas. An incisional biopsy was taken; cholecystectomy and T-tube drainage were performed. Biopsy showed a nonspecific inflammation and the patient was transferred to our clinic. In the laboratory tests; peripheral blood count results were in the normal range even eosinophil count, total bilirubin 1.75 mg/dL (0.2-1.0), direct bilirubin 0.80 mg/dL (0.0-0.3), alkaline phosphatase 254 U/L (30-135), AST 117 U/L (5-42), ALT 188 U/L (5-45), GGT 182 U/L (5-85). Tumor markers, CEA and CA 19-9, were in normal limits; 0.7 ng/mL (0-4) and 8.5 U/mL (3-35) respectively. A computed tomography-angiography revealed pancreatic head expansion particularly prominent at the uncinate process and no vascular invasion was detected (Figure 1). The abrupt termination of common bile duct at the T-tube cholangiography suggested a pancreas tumor (Figure 2). Pancreatoduodenectomy was performed and the patient was discharged on the 10th day of the operation without any problem. Gross examination of the specimen revealed a 3.5 cm lesion, pale and gray in color, in the head of the pancreas. Microscopic investigation demonstrated chronic atrophic pancreatitis with the findings of inflammation and ductal damage due to extensive eosinophilic infiltration. There was no eosinophilic infiltration in the common bile duct, stomach, duodenum and proximal jejunum. There was no malignancy at the histological examination (Figure 3). There was widespread eosinophilic infiltration on the surgical margins of the pancreas. No additional medical treatment required. She had no history of atopy. Colonoscopy was performed after her discharge and no inflammation was detected. With these clinical and histopathological finding the case was determined of “eosinophilic pancreatitis without systemic involvement”. For the following nine months, the patient didn’t experience any recurrent attacks of pancreatitis.
Discussion
Eosinophilic pancreatitis (EP) is a rare condition that usually presents with obstructive jaundice and it is most often diagnosed in the histopathological examination of the specimen after pancreatic resection for suspicion of malignancy [2-5]. EP may occur as a component of hypereosinophilic syndrome with eosinophilic infiltration of the gastrointestinal tract [4,6,7]. An allergic origin has been suggested in these cases [8,9]. Solitary eosinophilic infiltration of the pancreas is a very rare event. In this patient, the operative indication was a mass in the head of the pancreas causing biliary tract obstruction. Although an incisional biopsy taken at another hospital had shown no signs of malignancy. We concluded that a tumor obstructing the distal common bile duct couldn’t be ruled out. So, the true behavior was pancreatoduodenectomy. Histopathological examination displayed eosinophilic pancreatitis. There was no peripheral eosinophilia, nor eosinophilic infiltration in other resected organs. Since there is no pathognomonic radiological method to diagnose EP, a definitive diagnosis in preoperative period is difficult. In this case, young age of the patient and absence of weight loss were not features of a ductal adenocarcinoma of the pancreas. However, resection was justified, as it was not possible to rule out malignancy. Misdiagnosed benign pancreatic tumor resection incidence is reported to be around 5% [10,11]. By the use of recent diagnostic modalities such as MR pancreatography, endoscopic ultrasonography and biopsy under its guidance, could avoid unnecessary surgical procedures. However, routine use of EUS-guided biopsy for resectable pancreatic masses is controversial and American Gastroenterological Association recommends it only in unrespectable lesions [12]. Perhaps biopsy indications may be expanded in cases suspicious for benign tumors such as eosinophilic pancreatitis. Isolated eosinophilic infiltration of the pancreas is less than supposed and the other gastrointestinal organs must be detected for the involvement [3,5]. If a definitive diagnosis can be achieved before operative decision, the disease can be treated non-surgically. Bastid et al. reported a case treated successfully by sodium cromoglycate and another by prednisolone [9].
- Abraham SC, Leach S, Yeo CJ, Cameron JL, Murakata LA, et al. (2003) Eosinophilic pancreatitis and increased eosinophils in the pancreas. Am J Surg Pathol 27: 334-342. Link: https://tinyurl.com/y835lnl2
- Rakesh K, Banerjee R, Gupta R, Ramji C, Pradeep R, et al. (2006) Eosinophilic pancreatitis with pseudocyst. Indian J Gastroenterol 26: 136-137. Link: https://tinyurl.com/yah55s99
- Euscher E, Vaswani K, Frankel W (2000) Eosinophilic pancreatitis: a rare entity that can mimic a pancreatic neoplasm. Ann Diagn Pathol 4: 379-385. Link: https://tinyurl.com/y7zxd6u9
- Barthet M, Hastier P, Buckley MJ, Bernard JP, Sastre B, et al. (1998) Eosinophilic pancreatitis mimicking pancreatic neoplasia: EUS and ERCP findings--is nonsurgical diagnosis possible? Pancreas 17: 419-422. Link: https://tinyurl.com/y7ut4m8f
- Cay A, Imamoglu M, Cobanoglu U (2006) Eosinophilic pancreatitis mimicking pancreatic neoplasia. Can J Gastroenterol 20: 361-364. Link: https://tinyurl.com/yctzl4cj
- Hashimoto F (1980) Transient eosinophilia associated with pancreatitis and pseudocyst formation. Arch Intern Med 140: 1099-1100. Link: https://tinyurl.com/y7c4lhtp
- Tokoo M, Oguchi H, Kawa S, Homma T, Nagata A (1992) Eosinophilia associated with chronic pancreatitis: an analysis of 122 patients with definite chronic pancreatitis. Am J Gastroenterol 87: 455-460. Link: https://tinyurl.com/y8qswfjj
- Cromwell TA, Campbell DA (1971) Eosinophilic gastritis: a case report and etiological investigation. Surgery 69: 300-305. Link: https://tinyurl.com/y8qe7zhp
- Bastid C, Sahel J, Choux R, Payan MJ, Sarles H (1990) Eosinophilic pancreatitis: report of a case. Pancreas 5: 104-107. Link: https://tinyurl.com/yd48k3hz
- Smith CD, Behrns KE, van Heerden JA, Sarr MG (1994) Radical pancreatoduodenectomy for misdiagnosed pancreatic mass. Br J Surg 585-589. Link: https://tinyurl.com/y7658yvp
- van Gulik TM, Reeders JW, Bosma A, Moojen TM, Smits NJ, et al. (1997) Incidence and clinical findings of benign, inflammatory disease in patients resected for presumed pancreatic head cancer. Gastrointest Endosc 146: 417-423. Link: https://tinyurl.com/y9cjl886
- DiMagno EP, Reber HA, Tempero MA (1999) AGA technical review on the epidemiology, diagnosis, and treatment of pancreatic ductal adenocarcinoma. American Gastroenterological Association. Gastroenterology 117: 1464-1484. Link: https://tinyurl.com/ybxvogej

Article Alerts
Subscribe to our articles alerts and stay tuned.
 This work is licensed under a Creative Commons Attribution 4.0 International License.
This work is licensed under a Creative Commons Attribution 4.0 International License.
 Save to Mendeley
Save to Mendeley
