Journal of Gynecological Research and Obstetrics
Hysterotomy for Early Placenta Percreta at 10 Weeks Gestation: A Case Report
El-Said N1* and Kotb AM2
2Lecturer in Obstetrics and Gynecology, Ain Shams University, Cairo, Egypt
Cite this as
El-Said N, Kotb AM (2017) Hysterotomy for Early Placenta Percreta at 10 Weeks Gestation: A Case Report. J Gynecol Res Obstet 3(2): 034-036. DOI: 10.17352/jgro.000035Placenta percreta in early pregnancy is rare and only few cases are documented. We report a case of placenta percreta at 10 weeks gestation. Sonography revealed absence of line of demarcation between trophoblast and myometrium extending to the urinary bladder region. Termination of pregnancy by hysterotomy was done. The diagnosis and treatment of placenta accreta in early pregnancy must be taken seriously which might protect patients from considerable bleeding and further morbidity.
Case Report
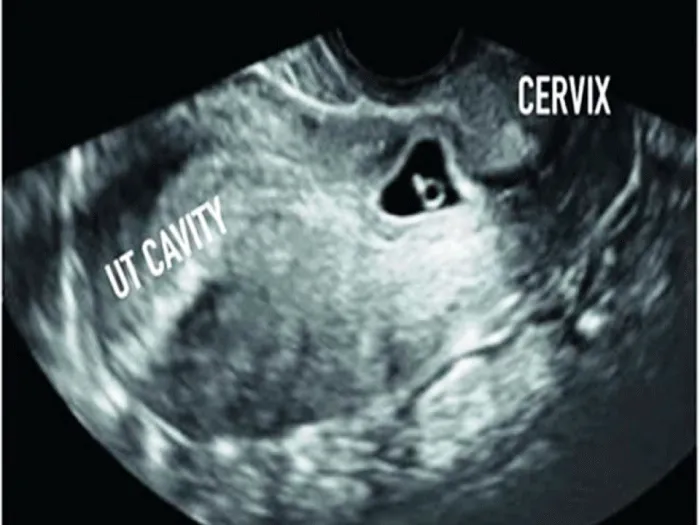
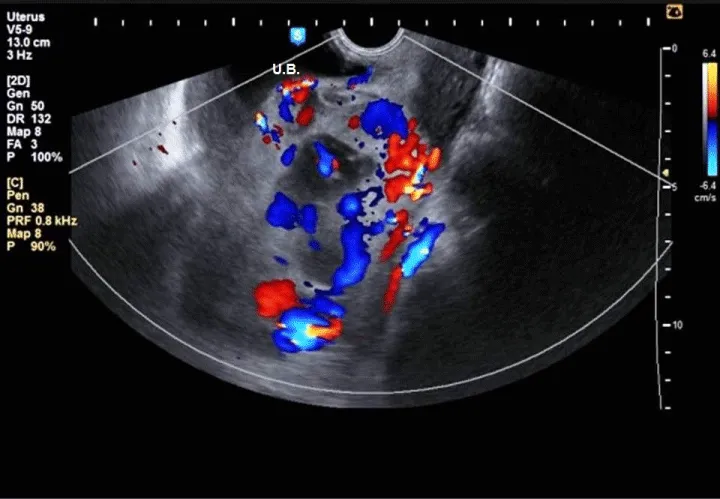
A 26 years old lady who had previously given birth to two children by cesarean sections (CS) and an exploratory laparotomy 10 years before marriage for removal of a complicated ovarian cyst. She was presented with a 2 weeks missed period where trans-vaginal ultrasound revealed a 5 weeks single intrauterine gestational sac equipping the isthmo-cervical portion of the uterus almost at site of the previous caesarean section scar with empty uterine cavity Figure 1. Two weeks later, the sac was still in the same site with positive fetal pulsation and another two weeks later, she started to develop mild vaginal bleeding with mild lower abdominal pain where ultrasound revealed healthy pregnancy with retro-chorionic hematoma 5 × 4 cm. 3 Dimension Ultrasound Doppler revealed the absence of demarcation line between trophoblast and myometrium with the trophoblast reaching as far as the serosa of the peritoneum covering the urinary bladder Figure 2. Termination of pregnancy by laparotomy was performed where the urinary bladder was found completely adherent to the uterus with high vascularity and varicosity covering this area. Bilateral uterine arteries ligation was done before opening the uterus. Small bladder injury occurred during dissection of the urinary bladder, which was sutured later on in double layer. On uterine incision, chorionic tissue was found bulging from site of the scar Figure 3 with a small part adherent to the uterine wall, excision of this part and closure of uterus was done after taking 3 U-shaped sutures in the lower part of the uterus. Patient received 2 units of blood and 2 units of plasma.
Discussion
Over the last few decades, CS rates have continued to rise [1]. The increasing CS rate stimulated the interest in potential long-term morbidity of CS scars [2].
Placenta accreta (and percreta) are not commonly diagnosed in the first trimester. They are usually diagnosed with the massive bleeding encountered during dilatation and curettage secondary to myometrial invasion by the placenta, unfortunately, a retrospective diagnosis [3]. The suspicion of placenta accreta developed in this case as early as the first ultrasound done showing a low lying gestational sac with empty uterus [2].
To our knowledge, over the past 20 years, the reported cases of placenta accreta diagnosed during the first trimester (≤ 12 weeks), were mostly discovered after the occurrence of severe bleeding either during an abortive curettage and/or during the post abortive weeks Table 1 [4]. This case was diagnosed pre-operatively with ultrasound and Doppler blood flow, with suspicion of percreta which was confirmed intra-operatively.
A low-lying gestational sac adherent to the anterior uterine wall needs to be differentiated from a low-lying sac that is surrounded equally by myometrium, both anteriorly and posteriorly. If cesarean section scar ectopic pregnancy is suspected in this gestational age, the use of methotrexate may be beneficial to avoid further complications like scar rupture or placenta accreta.
This diagnosis of placenta accreta (PA) is difficult during the first trimester, the currently known prenatal sonographic characteristics of PA low-lying gestational sac with diffuse dilatation of intra-placental vessels (lacunae). Also, PA is suspected if part of the lining of the gestational sac is embedded in the previous CS scar with an irregular decidual layer and thinning of the underlying uterine wall [5,6].
Hysterectomy has been the traditional treatment for PA with the idea that conservative treatment causes a four times higher mortality rate than treatment with an immediate hysterectomy [7]. However, there is only little experience concerning the treatment of the condition during first trimester; so, the choice between hysterectomy and conservative therapy should be dependent on the severity of bleeding.
Most of the reported cases have used hysterectomy as the standard line of treatment. Yang et al. 2009 [7] performed a ‘‘prophylactic’’ first trimester hysterectomy (at 12 weeks’ gestation) after diagnosis of low implanted PA in a 33-year-old woman, with a history of two previous CS. Bilateral uterine artery embolization was performed preoperatively to reduce expected bleeding during hysterectomy. Other reports indicated that conservative invasive procedures could be adapted to preserve fertility; these procedures included angiographic uterine artery embolization and laparoscopic or surgical resection of the affected area of the uterus [8].
Generally all these methods must be critically considered. In certain settings, uterine conservation, leaving the placenta in situ might be considered. Adjuvant therapy with methotrexate has also been described to expedite the placental resorption [9].
A reduction from 85% to 15% in hysterectomy rates was found that when placental retention was allowed. Morbidities associated with leaving the placenta in situ mainly included infection and coagulation disorder, which may necessitate subsequent hysterectomy [10].
In this case, we adopted early conservative invasive management during early trimester where the patient’s conditions are stable to avoid possible excessive bleeding and high risk for hysterectomy later on and to avoid further possible bladder invasion.
In conclusion, detailed sonographic examination with high suspicion of PA should be considered for women at risk during the first trimester. Early diagnosis may allow earlier elective intervention that decreases maternal morbidity and mortality. Considering the rising rate of CS, the incidence of PA in early gestation will increase. So, clear evidence guiding the screening, diagnosis and management of this condition is needed.
- Betran AP, Merialdi M, Lauer JA, Bing-Shun W, Thomas J, et al. (2007) Rates of caesarean section: analysis of global, regional and national estimates. Paediatr Perinat Epidemiol 21: 98-113. Link: https://goo.gl/qtmStH
- Clark EA, Silver RM (2011) Long-term maternal morbidity associated with repeat cesarean delivery. Am J Obstet Gynecol 205: S2-10. Link: https://goo.gl/N368jS
- Hopker M, Fleckenstein G, Heyl W, Sattler B, Emons G (2002) Placenta percreta in week 10 of pregnancy with consecutive hysterectomy: case report. Hum Reprod 17: 817-820. Link: https://goo.gl/vV9psE
- Shaamash AH, Houshimi WM, El-kanzi EM, Zakaria AE (2014) Abortion hysterectomy at 11 weeks’ gestation due to undiagnosed placenta accreta (PA): A case report and a mini review of literatures. Middle East Fertility Society Journal 19: 147-152. Link: https://goo.gl/0KOubf
- Shih JC, Cheng WF, Shyu MK, Lee CN, Hsieh FJ (2002) Power Doppler evidence of placenta accretaappearing in the first trimester. Ultrasound Obstet Gynecol 19: 623-625. Link: https://goo.gl/nG6tVf
- Wong HS, Zuccollo J, Tait J, Pringle KC (2009) Placenta accreta in the first trimester of pregnancy: sonographic findings. J Clin Ultrasound 37:100-103. Link: https://goo.gl/ZtUSVC
- Yang JI, Kim HY, Kim HS, Ryu HS (2009) Diagnosis in the first trimester of placenta accreta with previous Cesarean section. Ultrasound Obstet Gynecol 34: 116-118. Link: https://goo.gl/uIIsQK
- Wang YL, Su TH, Huang WC, Weng SS (2011) Laparoscopic management of placenta increta after late first-trimester dilation and evacuation manifesting as an unusual uterine mass. J Minim Invasive Gynecol 18: 250-253. Link: https://goo.gl/cIjQTp
- Hunt JC (2010) Conservative management of placenta accreta in a multiparous woman. J Pregnancy 2010: 329618. Link: https://goo.gl/GvW5o2
- Kayem G, Davy C, Goffinet F, Thomas C, Clement D, et al. (2004) Conservative versus extirpative management in cases of placenta accreta. Obstet Gynecol 104: 531-536. Link: https://goo.gl/iowsDz
Article Alerts
Subscribe to our articles alerts and stay tuned.
 This work is licensed under a Creative Commons Attribution 4.0 International License.
This work is licensed under a Creative Commons Attribution 4.0 International License.


 Save to Mendeley
Save to Mendeley
