Journal of Gynecological Research and Obstetrics
Multi Centric Paget’s Disease and Review of Literature
Zohreh Yousefi1, Marjaneh Farazestanian2, Amir Hosein Jafarian3, Laya Shirinzadeh4* and Anahita Hamidi5
2Department of Gynecology, Mashhad University of Medical Sciences, Ghaem Hospital, Faculty of Medicine, Mashhad, Iran
3Department of Pathology, Mashhad University of Medical Sciences, Anatomo clinical Pathologist, Associated professor, Ghaem Hospital, Faculty of Medicine, Mashhad, Iran
4Department of Obstetrics and Gynecology, Mashhad University of Medical Sciences, Resident Fellowship of Gynecology Oncology, Ghaem Hospital, Faculty of Medicine, Mashhad, Iran
5Department of Obstetrics and Gynecology, Mashhad University of Medical Sciences, Resident of Gynecology Oncology, Ghaem Hospital, Faculty of Medicine, Mashhad, Iran
Cite this as
Yousefi Z, Farazestanian M, Jafarian AH, Shirinzadeh L, Hamidi A (2017) Multi Centric Paget’s Disease and Review of Literature. J Gynecol Res Obstet 3(1): 005-007. DOI: 10.17352/jgro.000028Introduction: Paget’s disease of the vulva (PDV) is a very rare malignancy originating in vulvar apocrine-gland-bearing skin cells. Based on multi centric nature of Paget’s disease, it’s a chronic and relapsing course. The aim of this report is to introduce a case of multi centric Paget’s disease and review of literature.
Case report: A 62-year-old woman with complaints of vulvar pruritus, painful vulvar lesion for 4 years was referred to oncology department of Ghaem hospital, Mashhad University of Medical Sciences in 2016. Pathological results of erythematous and exfoliated lesion of the major and minor labia extend to anus was reported as PDV with full-thickness involvement. In investigations, she had persistent hematuria. Pelvis and abdomen investigation revealed irregularity in the posterior wall of the bladder and biopsy detected urothelial carcinoma in the bladder. Radical cystectomy was performed subsequently. In addition, complete response of vulvar lesion to imiquimod cream was seen after 6 weeks of therapy. The patient is free of disease and now she is under serial follow-up.
Conclusion: Generally standard treatment modality in patients who experienced multicenteric Paget’s disease is surgical resection, also topical 5% imiquimod cream may be considered as an alternative option in setting metastatic vulvar Paget.
Introduction
Paget’s disease of the vulva (PDV) is an extremely rare intraepithelial neoplasm, accounting for only 1% of vulvar malignancies [1]. Based on origin of neoplastic paget cells in the classification system of WiIkinson and Brown, two types of PDV, primary and secondary disease has proposed. Primary cutaneous Paget’s disease, an intraepithelial adenocarcinoma, arises within the epidermis or underlying skin appendages. Secondary or non-cutaneous Paget’s disease originates from an underlying non-cutaneous adenocarcinoma. Most commonly anorectal adenocarcinoma, urothelial carcinoma (bladder or urethra), carcinoma of the cervix [2]. 10% of patients with Paget’s disease of the vulva have an underlying second malignancy. A diagnostic biopsy and immunohistochemical studies may be of great use in distinguishing primary and secondary lesions [3]. The most common presenting complaint and clinical manifestation of patients are well-demarcated, thickened, pruritic, erythematous, or white scaly plaque with irregular borders commonly develop in postmenopausal women. The patient always suffers for several years before seeking medical advice [4]. In Japanese study, Paget’s disease of the vulva was seen 5 years later than the onset of the disease and 87.5% of patients suffer of vulvar eczematous change with itching [5]. Standard treatment of PDV is surgical excision. Preoperational evaluation of these lesions is important, because 20-30% of cases have an underlying malignancy [6]. Wong et al., reported that 26% of the women had underlying adenocarcinoma, and twenty-two percent of cases had additional malignancies at other sites, which is consistent with other reports [7]. Over the years, many therapeutic modalities have been attempted on patients with PDV in an effort to reduce the significant morbidity associated with the after-radical surgical treatments [8]. Because of the rarity of this disease, we report a case of multi centric Paget’s disease and review of literature.
Case Report
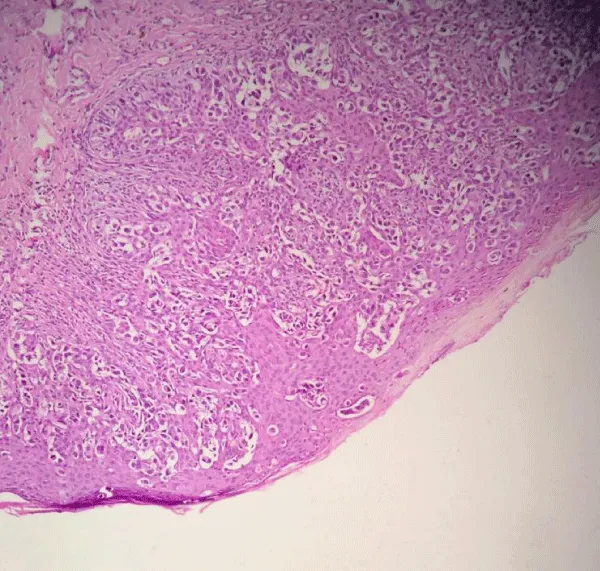
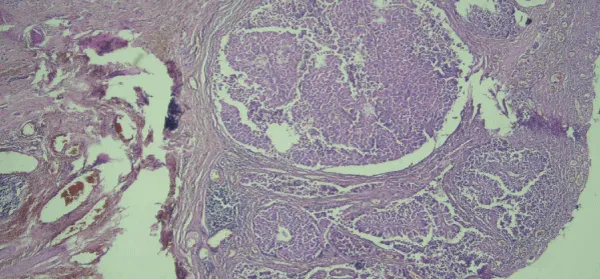
A 62-years old female was in natural menopause for 14 years. She was referred to oncology department of Ghaem hospital, Mashhad University of Medical Sciences in July 2016. She suffered of painful vulvar lesion with severe purities for 4 years. In examination, an erythematous and exfoliated lesion of the right major and minor labia extend to anus was detected. It also extended up to the clitoris, but did not invade to external urethral meatus. She had history of using recurrent topical corticosteroid. The result of the biopsy was PDV with full-thickness involvement (Figure 1). In investigations, she had persistent hematuria. Screened for any associated underlying malignancies including breast examination, mammography, pelvic and abdominal ultrasonography, colonoscopy, and chest X-ray were normal. Pelvic CT scan was revealed irregularity of the posterior wall of the bladder. Results of cystoscopy biopsy determined low-grade urothelial carcinoma (Figure 2). As an associated malignancy, she underwent successful radical cystectomy. In addition, treatment proposed for the vulvar lesion topical imiquimod 5% cream to be applied every other day after confirming of bladder carcinoma. After 6 weeks of therapy, the patient is free of disease and now is under serial follow-up.
This paper has been performed according to patient’s informed consent.
Discussion
In patients with PDV, higher rate of underlying adenocarcinoma was observed; like our patient who had bladder carcinoma, but her manifestation was PDV. The most common site of involvement up to 60% of Paget’s disease is the vulva [9]. All patients with PDV have poor outcomes and should be screened for any associated malignancies. The investigations should include mammography, CT scan of the pelvis and abdomen, trans-vaginal ultrasonography, and cervical cytology. Colonoscopy should be undertaken if the lesion involved the anus, while if the urethra is involved, cystoscopy is indicated [10]. Investigation in our patient revealed bladder carcinoma. The median interval from the onset of symptoms to a histological diagnosis was approximately 20 months, which suggests that the disease is slowly progressive [11]. We had delayed diagnosis of 4 years in this patient. Many patients undergo multiple surgical procedures, including wide local excision with a gross margin of 2-3 cm which is confirmed by frozen section analysis. However, margins of primary surgical specimens are positive in more than half of the patients, so careful attention should be undertaken during surgery [12]. Also, because the disease usually extends well beyond the gross lesion, resection of the fascia must be keeping in mind. In addition, simple or radical vulvectomy may be considered. Consequently, limiting resection in favor of the preservation of the clitoris, urethra, and anus is recommended [13]. However, underlying carcinoma in our patient influenced in medical treatment of PDV. Due to the high morbidity, side-effects, local failure and frequent recurrences of surgical treatment, nonsurgical therapy has been proposed. These modality treatments include topical photodynamic therapy, fluorouracil (5-Fu), and 5% imiquimod cream that lead to effective results. Also, regardless of the involved area, clinical response, symptom control and preserving cosmetic features was obtained. Also in a meta-analysis study in Cochrane they not agree with any interventions after treatment of PDV in prevent of recurrence [14]. In our patient, due to waiting time for treatment of bladder carcinoma , since PDV was metastases of this cancer, topical therapy was applied, so we are unable to compare these two methods of therapy. Mostly invasion of adjacent organ due to metastases of bladder carcinoma was occurred in direct invasion by tumors. Above mentioned, the involving vulva (Paget’s disease) as a metastatic lesion of bladder carcinoma may be occurred; also it is very rare. Hence, in the management of PDV, long-term monitoring of patients is recommended and repeat surgical excision is often necessary [15]. The optimum treatment regimen needs to be investigated in future prospective studies.
Conclusion
Generally standard treatment modality in patients who experienced multi centeric Paget’s disease is surgical resection, but topical 5% imiquimod cream should be considered as An alternative to surgical treatment including of the vulva.
- Jones IS, Crandon A, Sanday K (2011) Paget’s disease of the vulva: diagnosis and follow up key to management; a retrospective study of 50 cases from Queensland. Gynecol Oncol 122: 42-44. Link: https://goo.gl/Zr8ZSa
- Shaco-Levy R, Bean SM, Vollmer RT, Papalas JA, Bentley RC, et al. (2010) Paget disease of the vulva: a histologic study of 56 cases correlating pathologic features and disease course. Int J Gynecol Pathol 29: 69-78. Link: https://goo.gl/P8LGS2
- Lopes, Filho LL, Lopes IM, Lopes LR, Enokihara MM, Michalany AO, et al. (2015) Mammary and extramammary Paget’s disease. An Bras Dermatol 90: 225-231. Link: https://goo.gl/Ds56H9
- Lam C, Funaro D (2010) Extramammary Paget’s disease: summary of current knowledge. Dermatol Clin 28: 807-826. Link: https://goo.gl/8SV2Os
- Jiang H, Ma C, Guo S (2016) Management of vulvar Paget’s disease: a case report and review of the literature. Int J Clin Exp Med 9: 12323-12327. Link: https://goo.gl/D88OgS
- Cai Y, Sheng W, Xiang L, Wu X, Yang H (2013) Paget’s disease the vulva: The clinicopathological features and treatment outcomes in a series of 43 patients. Gynecol Oncol 129: 412-416. Link: https://goo.gl/10Xs2T
- Wong SM, Freedman RA, Stamell E, Sagara Y, Brock JE, et al. (2015) Modern Trends in the Surgical Management of Paget’s Disease. Ann Surg Oncol 22: 3308-16. Link: https://goo.gl/o3mAJL
- Ellis PE, Maclean AB, Wong LF, Fong T, Crow JC, et al. (2012) Angiogenesis in Paget’s disease of the vulva and the breast: correlation with microvessel density. J Oncol 2012: 651507. Link: https://goo.gl/zHcfw3b
- Karam A, Dorigo O (2012) Treatment outcomes in a large cohort of patients with invasive Extramammary Paget's disease. Gynecol Oncol 125: 346-351. Link: https://goo.gl/7ObqLj
- Reyes MC, Park KJ, Lin O, Ioffe O, Isacson C (2012) Urothelial carcinoma involving the gynecologic tract: a morphologic and immunohistochemical study of 6 cases Am J Surg Pathol 36: 1058-1065. Link: https://goo.gl/E1IuNk
- Simon SK, Bolanca IK, Sentija K, Kukura V, Valetić J (2010) Vulvar Paget's disease-a case report. Coll Antropol 34: 649-52. Link: https://goo.gl/DVsg8d
- Cowan RA, Black DR, Hoang LN, Park KJ, Soslow RA, et al. (2016) A pilot study of topical imiquimod therapy for the treatment of recurrent extramammary Paget's disease. Gynecol Oncol 142: 139-143. Link: https://goo.gl/Z3pnd1
- Fontanelli R, Papadia A, Martinelli F, Lorusso D, Grijuela B, et al. (2013) Photodynamic therapy with M-ALA as nons urgical treatment option in patients with primary extramammary Paget's disease. Gynecol Oncol 130: 90-94. Link: https://goo.gl/yCAXYA
- Machida H, Moeini A, Roman LD, Matsuo K (2015) Effects of imiquimod on vulvar Paget's disease: A systematic review of literature. Gynecol Oncol 139: 165-171. Link: https://goo.gl/DZottK
- Jones IS, Crandon A, Sanday K (2011) Paget's disease of the vulva: Diagnosis and follow-up key to management A retrospective study of 50 cases from Queensland. Gynecol Oncol 122: 42-44. Link: https://goo.gl/35tYXY
Article Alerts
Subscribe to our articles alerts and stay tuned.
 This work is licensed under a Creative Commons Attribution 4.0 International License.
This work is licensed under a Creative Commons Attribution 4.0 International License.

 Save to Mendeley
Save to Mendeley
