Journal of Gynecological Research and Obstetrics
A Case of Severe, Silent Fetomaternal Haemorrhage (FMH) Detected by Mixed-Field in the Mother’s ABO Typing
Aurora Espinosa1*, Kristin Finserås1, Grete Storvold1, Tone Wedø1, Kristin Fonn1, Seema Mathew2, Eline B Seljeflot2 and Eszter Vanky2
2Department of Gynecology, St. Olav’s University Hospital, Trondheim, Norway
Cite this as
Espinosa A, Finserås K, Storvold G, Wedø T, Fonn K, et al. (2016) A Case of Severe, Silent Fetomaternal Haemorrhage (FMH) Detected by Mixed-Field in the Mother’s ABO Typing. J Gynecol Res Obstet 2(1): 061-062. DOI: 10.17352/jgro.000021Introduction: Fetomaternal haemorrhage (FMH) refers to the passage of fetal erythrocytes to the maternal circulation. In most pregnancies, small amounts of fetal erythrocytes can cross over to the maternal circulation without causing problems for the fetus. In rare occasions, the FMH can result in fetal anaemia or in fetal death.
Case report: Here, we present a case where a 30-year-old, II gravida, I para, in gestational week 35 reported decreased fetal movements, leading to the diagnosis of severe FMH. The fetal haemorrhage calculated by Kleihauer-Betke test was estimated to 287 mL, causing a mixed-field in the mother’s ABO typing, as the mother and the baby had different blood types. Fetal anaemia was suspected and diagnosed by Doppler ultrasound, and emergency caesarean section was performed, saving the baby’s life.
Discussion: Severe FMH is very rare, and may present as decreased fetal movements, together with sinusoidal fetal heart rate pattern. This condition requires rapid intervention such as intrauterine transfusions or emergency caesarean section. Assessment of fetal anaemia by Doppler ultrasound should be considered in mothers reporting decreased fetal movements.
Abbreviations
FMH: Fetomaternal Haemorrhage; KB: Kleihauer-Betke test; HbF: Fetal Haemoglobin; HbA: Adult Haemoglobin
Introduction
Small amounts of fetal erythrocytes may enter the maternal circulation in most pregnancies. The volume of such fetomaternal haemorrhage (FMH) is usually small (less than 1 mL in 96 percent of the pregnancies) and without clinical significance [1]. The cut-off volume for clinically significant FMH has been defined as >30 mL, occurring in approximately 3 out of 1000 pregnancies [2], and used as the threshold for the administration of anti-D prophylaxis, for the prevention of anti-D immunisation in Rh incompatible pregnancies. Severe FMH (>150 mL) leading to fetal anaemia, hydrops or stillbirth is relatively uncommon [3] and may present as decreased fetal movements, sinusoidal heart rate pattern, or fetal abnormalities [4]. Massive FMH may rarely occur without any predisposing event [5]. The ethology of FMH is unknown but it is thought to be multi-factorial. Stillbirth, neonatal anaemia, cephalic version, abdominal trauma, preeclampsia, amniocentesis and caesarean delivery have been correlated to the presence of fetal erythrocytes in the maternal circulation [6]. The Kleihauer-Betke (KB) acid elution test is used to estimate the amount of fetal erythrocytes in maternal circulation. The test is based on the principle that fetal erythrocytes, containing fetal hemoglobin (HbF), are resistant to acid elution, while adult erythrocytes containing adult Hb (HbA) are sensitive. A formula is used to calculate the estimated amount of FMH, based on the number of fetal cells found. Although the Kleihauer-Betke test requires no special equipment, it is time-consuming and lacks standardization and precision [7]. In the last decade, flow cytometry analysis has been developed to detect HbF and/or anti-D. Flow cytometry correlates well with KB test and it is considered the gold standard for the quantification of FMH [8].
Case Presentation
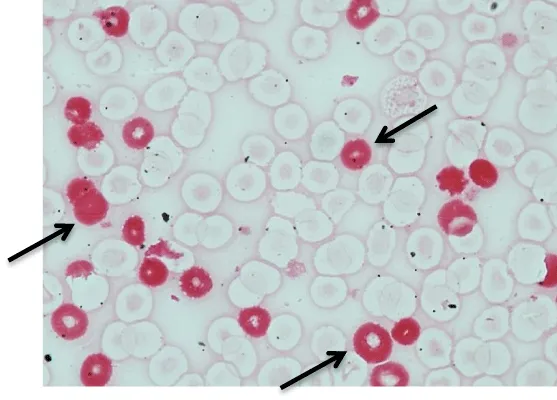
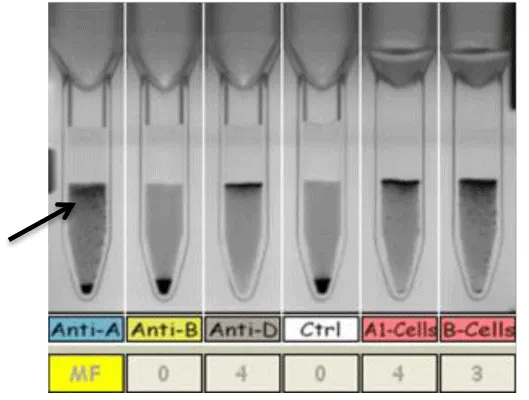
We present a case where a 30-year-old, gravida II, para I woman, with blood group 0 Rh D+ was admitted to the hospital at gestational week 35 due to reduced fetal movements. There was no known history of trauma, invasive procedures or other predisposing factors during pregnancy. The mother’s ABO typing showed mixed field when her erythrocytes were typed with anti-A (Figure 1), indicating the presence of blood group A fetal erythrocytes, together with the maternal, group O erythrocytes. The mother had not received any blood transfusion which could have explained the presence of group A erythrocytes in her circulation. Ultrasound examination revealed reduced amniotic fluid, estimated fetal growth restriction (-16% of the estimated weight at 35th gestational week) and increased median cerebral artery blood flow (Figure 2), indicating a distressed fetus with possible anaemia. A baby boy was delivered by caesarean section the same day. He was limp, pale and weighed 1954 g corresponding to -30% growth restriction, with Apgar score 6 and 7 at 5 and 10 minutes respectively. The baby’s haemoglobin level was 2.7 g/dL. Fetomaternal haemorrhage (FMH) was confirmed by the presence of fetal erythrocytes in the maternal circulation by the KB-test drawn before delivery (Figure 3). The amount of fetal erythrocytes in the maternal circulation was estimated to 287 mL, which was interpreted as either a chronic, slow bleeding over time or recurrent rapid blood loss. Macroscopic assessment of the placenta showed no pathology. Microscopic examination showed the presence of nucleated erythrocytes in fetal circulation, consistent with fetal anaemia. The mother’s hemoglobin level was 13.2 g/dL before delivery. Peri- and post-operative bleeding was estimated to 450 mL, and no extensive fluid replacement was given. Two days postpartum, her haemoglobin level was 9.8 g/dL, which may indicate a possible maternal haemolysis, due to the presence of high level of ABO- incompatible fetal red blood cells.
The baby received several transfusions after birth. At the age of 8 months, he was considered healthy and normally developing.
Discussion
Massive FMH may occur without any clinical history of trauma. As presented in this case, fetal anaemia was suspected due to reduced fetal movements, reported by the mother. In this case, the timing of the FMH is difficult to determine, but it probably occurred over a long period, making it possible for the fetus to “adapt”. A rapid intervention with caesarean section saved the baby’s life. Mixed-field in the maternal ABO typing was due to the different maternal and fetal ABO blood types, and illustrates the degree of FMH. Only the KB test was performed to detect fetal erythrocytes in the maternal circulation, as flow cytometric measurement of FMH is not available at our department.
Conclusion
In conclusion, we present a case of severe, silent FMH diagnosed at gestational week 35, where the only clinical sign was decreased fetal movements reported by the mother. FMH may be difficult to suspect, in the absence of predisposing factors. This case supports the importance of awareness of reduced fetal movements in late pregnancy. The prompt examination by Doppler ultrasound revealed severe anaemia in the baby, and emergency caesarean section followed by blood transfusions in the postnatal period saved the baby’s life.
- Bowman, JM, Pollock JM, Penston LE (1986) Fetomaternal transplacental hemorrhage during pregnancy and after delivery. Vox Sang 51: 117-121 .
- Sebring ES, Polesky HF (1990) Fetomaternal hemorrhage: incidence, risk factors, time of occurrence, and clinical effects. Transfusion 30: 344-357 .
- O'Leary BD, Walsh CA, Fitzgerald JM, Downey P, McAuliffe FM (2015) The contribution of massive fetomaternal hemorrhage to antepartum stillbirth: a 25-year cross-sectional study. Acta Obstet Gynecol Scand 94: 1354-1358 .
- Pourbabak S, Rund CR, Crookston KP (2004) Three cases of massive fetomaternal hemorrhage presenting without clinical suspicion. Arch Pathol Lab Med 128: 463-465 .
- Samadi R, Greenspoon JS, Gviazda I, Settlage RH, Goodwin TM (1999) Massive fetomaternal hemorrhage and fetal death: are they predictable? J Perinatol 19: 227-229 .
- Wylie BJ. D´Alton ME (2010) Fetomaternal Hemorrhage. Obstet Gynecol 115: 1039-1051 .
- Kim YA, Makar RS (2012) Detection of fetomaternal hemorrhage. Am J Hematol 87: 417-423 .
- Chambers E, Davies L, Evans S, Birchall J, Kumpel B (2012) Comparison of haemoglobin F detection by the acid elution test, flow cytometry and high-performance liquid chromatography in maternal blood samples analysed for fetomaternal haemorrhage. Transfus Med 22: 199-204 .
Article Alerts
Subscribe to our articles alerts and stay tuned.
 This work is licensed under a Creative Commons Attribution 4.0 International License.
This work is licensed under a Creative Commons Attribution 4.0 International License.


 Save to Mendeley
Save to Mendeley
