International Journal of Clinical Endocrinology and Metabolism
Free Triiodothyronine Toxicosis in Adolescent Monozygotic Twin Brothers
1Medical University of Warsaw, Warsaw, Poland
2Department of Family Medicine, Medical University of Warsaw, Warsaw, Poland
3Department of Family Medicine, National Medical Institute of the Ministry of Interior and Administration, Warsaw, Poland
4Department of Rheumatology, Systemic Connective Tissue Diseases and Rare Diseases, National Medical Institute of the Ministry of Interior and Administration, Warsaw, Poland
Author and article information
Cite this as
Kuncewicz M, Szydlarska D, Ciechomska M, Życińska K. Free Triiodothyronine Toxicosis in Adolescent Monozygotic Twin Brothers. Int J Clin Endocrinol Metab. 2025; 11(1): 001-003. Available from: 10.17352/ijcem.000063
Copyright License
© 2025 Kuncewicz M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.Free triiodothyronine toxicosis is a rare condition, expressed by isolated triiodothyronine concentration elevation, resulting in an overt hypermetabolic state. Diagnosis and treatment are particularly important in young populations during puberty, with intensive intellectual and physical development. We present a case of monozygotic adolescent male twins, with cardiovascular symptoms, along with anxiety, hypersensitivity and insomnia. The free triiodothyronine toxicosis in the absence of anti-thyroid antibodies. Successful treatment with symptom relief and laboratory results normalization was achieved after 8 weeks of anti-thyroid medication with beta-blocker addition. The described condition may be an early stage of developing disease, so further follow-up is obligatory. Because the case presents an atypical population for the disorder, with brothers additionally being monozygotic twins, genetic factors should be taken into consideration in the event of disease progression.
Thyroid dysfunction is a frequent condition and the most common first-step laboratory tests in Poland are Free Thyroxine (FT4), Free Triiodothyronine (FT3), and Thyrotropin (TSH) levels, in some cases extended to autoantibodies panel [1]. Typically, in primary hyperthyroidism, FT4 and FT3 are elevated resulting in TSH suppression. In some cases, FT4 level remains normal, with only FT3 concentration elevated, which in association with clinical symptoms and absence of Thyroxine-binding Globulin (TBG) abnormalities, is referred to as FT3 toxicosis (FT3t) [2]. This hormonal dysregulation plays a key role in the development of thyrotoxicosis. Although FT4 concentration is significantly higher, it is regarded as a prohormone with limited direct activity [3]. To exert its effect, FT4 must be transported into target cells and then converted into the active molecule, FT3 [4]. Available data on FT3t remains limited and somewhat controversial. Therefore, this study is timely and important.
The aim of our study was to describe peculiarities of cardiological and psychiatric symptoms of FT3t syndrome. The patient’s consent for the study and its publication was obtained.
Case presentation
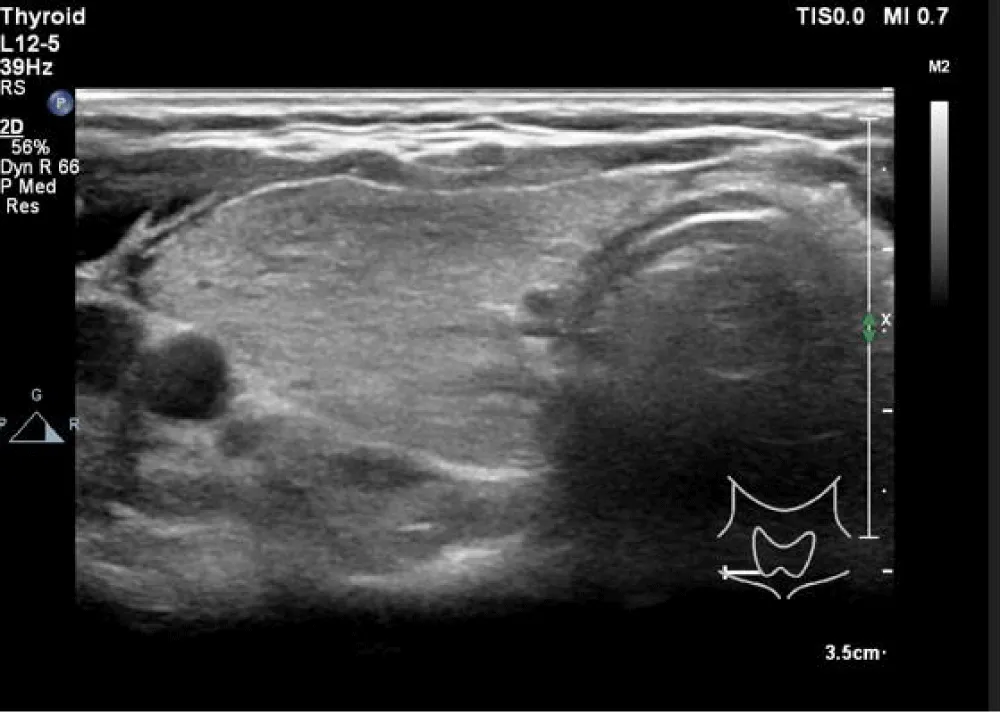
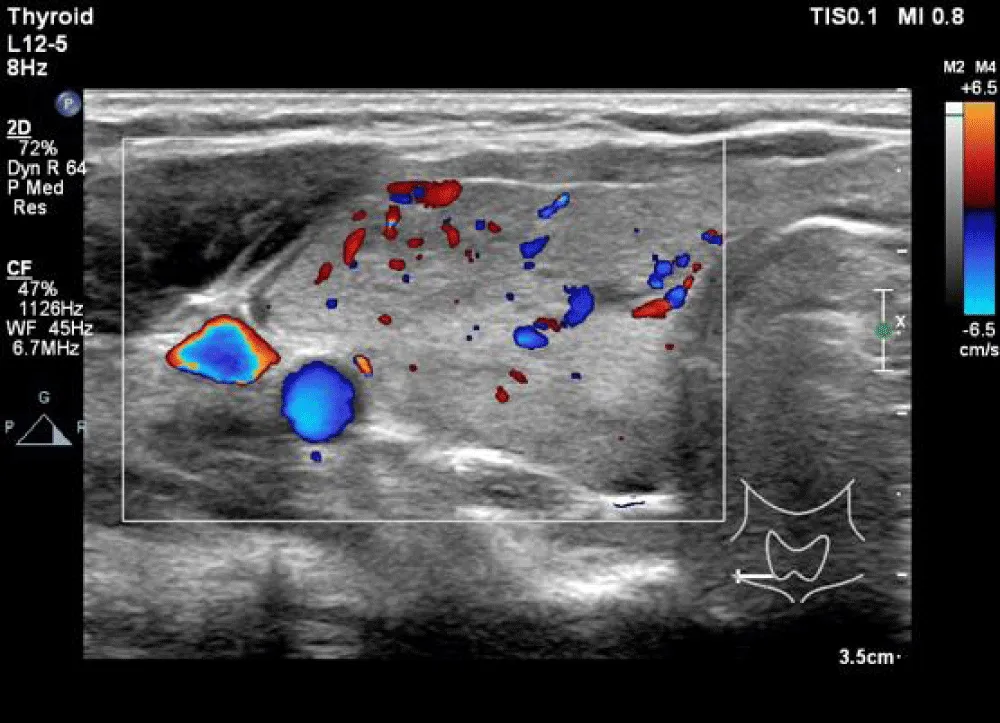
Sixteen-year-old monozygotic twin brothers, both regularly engaged in sports activities, were admitted to the Department of Endocrinology . As they were underage, they were accompanied by their mother. The main complaints were Cardiological symptoms such as heart rhythm disturbances, palpitations, and chest pain. A cardiology examination performed a few weeks earlier concluded with a diagnosis of sinus tachycardia. Additional abnormalities were hypersensitivity, anxiety attacks and insomnia. A physical examination was performed, and only tachycardia and hands tremor were observed. Laboratory findings (Table 1) revealed elevated FT3, with normal TSH and FT4 concentrations in both cases. Anti-thyroid antibodies were not detected. In both cases, liver and kidney function disorders were excluded, and blood glucose levels were normal. Additionally, an ultrasound examination of the thyroid gland was performed. The ultrasound findings were similar in both cases. The thyroid gland was described as normal in size and in the typical anatomical position. The echogenicity of the thyroid’s parenchyma was decreased, and somewhat heterogeneous, with slightly increased vascular flow. The cervical lymph nodes were not enlarged (Figures 1,2). Additionally, in one of the brothers, a physical examination revealed a mild bilateral gynecomastia without galactorrhoea. Sexual development was appropriate for the patient’s age. After excluding abnormalities in hormonal tests, pubertal gynecomastia was diagnosed.
Treatment with an antithyroid drug and a beta-blocker was implemented. During a follow-up visit after 8 weeks of therapy, a significant improvement in the general condition was observed, no tachycardia was noted, sleep improved, and a reduction in nervousness was reported. Laboratory tests showed features of euthyroidism.
Discussion
The prevalences of all-cause thyrotoxicosis and subclinical hyperthyroidism among adolescents are 0.04% and 4.4% respectively, with the overall hyperthyroidism female-to-male ratios increasing with age, from 1.43:1 among children under 5 years, surpassing 5:1 in the 15 to 17 years age population [5,6]. FT3t is a rare form of hyperthyroidism, with prevalence varying between studies and populations, reaching up to 16% of cases, which makes the described adolescent twins atypical patients [7]. Some authors differentiate FT3t into two subgroups: patients with elevated both FT3 and total triiodothyronine levels, and those with isolated FT3 concentration abnormality. No clinical significance has been attributed to this distinction, suggesting it remains a purely academic classification. Both conditions appear to represent early stages within the spectrum of thyroid hyperfunction disorders and are managed using the same therapeutic approaches [8].
The brothers presented mostly cardiovascular symptoms and disturbances in their mental condition. Cardiovascular problems are especially alarming and threatening, as some rare but serious heart diseases manifest at this age [9]. Unrecognized heart disease may present similarly, in extreme cases leading to sudden cardiac death e.g., during sports activities [10]. Therefore, a prompt differential diagnosis should always be conducted when symptoms are reported. Mental issues naturally lead to consultation with a psychologist or psychiatrist. Those specialists need to remember that presented problems can arise from organic diseases, and in reverse, specialists in somatic diseases cannot disregard psychological symptoms. Anxiety is a serious problem that may have a significant impact on adolescents’ behaviour, and thus their peer relations. Young people are more susceptible to the opinions of others and rely on social acceptance, making it particularly important to identify the problem early and initiate appropriate treatment [11]. Conversely, aggravation may lead to other serious psychiatric problems and impair psychosocial development [12,13]. Typical anxiety treatment, based on psychotherapy supported by pharmacotherapy, would be an inappropriate option in this case. Since an organic disease has triggered the symptoms, the primary treatment should focus on normalizing the FT3 concentration [14].
In both cases, ultrasound examination revealed normal size thyroid, with heterogenous echogenicity and increased blood flow. These findings are typically associated with systemic thyroid disease, such as Graves’ Disease (GD), the most common aetiology of hyperthyroidism in adolescents [15]. Although anti-TSH receptor antibodies (TRAb) were absent, but up to 18% of GD cases present in TRAb-negative form, often manifesting as a milder form of the disease [16,17]. Considering that FT3t can be an early stage of developing disease, it is possible, that in time TRAb will become positive, leading to classic GD, or patients may be diagnosed with antibodies negative GD form, or a completely different diagnosis is going to be set.
Although rare, accounting for < 5% of TRAb-negative hyperthyroidism, yet important to remember in the case of monozygotic twins, with identical genomes, there are genetic causes, such as TSH Receptor mutations and diseases [18,19]. However, since the response to the treatment was satisfactory, and the thyroid function abnormalities were isolated, further diagnosis was not necessary. Thyroid function was successfully stabilized; therefore, ongoing therapy and routine follow-up, including laboratory assessments and ultrasound evaluations are considered sufficient.
Pubertal gynecomastia is an incidental finding with no impact on further clinical management. It is a common reaction to hormonal changes and usually does not need any kind of treatment as the changes regress spontaneously [20].
- Lewiński A, Stasiak M. Cooperation between primary care physician and endocrinologist in the diagnosis and treatment of endocrinopathies. Primary Care Physician. 2017;3(2):73-90. Available from: https://www.termedia.pl/Wspoldzialanie-lekarza-POZ-i-endokrynologa-w-zakresie-diagnostyki-i-leczenia-endokrynopatii,98,29947,1,0.html
- Bahn Chair RS, Burch HB, Cooper DS, Garber JR, Greenlee MC, Klein I, et al. Hyperthyroidism and other causes of thyrotoxicosis: management guidelines of the American Thyroid Association and American Association of Clinical Endocrinologists. Thyroid. 2011;21(6):593-646. Available from: https://doi.org/10.1089/thy.2010.0417
- Galton VA. The ups and downs of the thyroxine pro-hormone hypothesis. Mol Cell Endocrinol. 2017;458:105-111. Available from: https://doi.org/10.1016/j.mce.2017.01.029
- Brent GA. Mechanisms of thyroid hormone action. J Clin Invest. 2012;122(9):3035-3043. Available from: https://doi.org/10.1172/jci60047
- Chen J, Zhang L, Zhang X. Overall, sex-and race/ethnicity-specific prevalence of thyroid dysfunction in US adolescents aged 12-18 years. Front Public Health. 2024;12:1366485. Available from: https://doi.org/10.3389/fpubh.2024.1366485
- Simon M, Rigou A, Le Moal J, Zeghnoun A, Le Tertre A, De Crouy-Chanel P, et al. Epidemiology of childhood hyperthyroidism in France: A nationwide population-based study. J Clin Endocrinol Metab. 2018;103(8):2980-2987. Available from: https://doi.org/10.1210/jc.2018-00273
- Snabboon T, Sridama V, Sunthornyothin S, Suwanwalaikorn S, Vongthavaravat V. A more appropriate algorithm of thyroid function test in diagnosis of hyperthyroidism for Thai patients. J Med Assoc Thai. 2004;87 Suppl 2:S19-21. Available from: https://pubmed.ncbi.nlm.nih.gov/16083155/
- Kazanavičius G, Lasaite L, Grazienė A. Syndrome of isolated FT3 toxicosis: A pilot study. J Clin Endocrinol Metab. 2012;3:1-5. Available from: https://academicjournals.org/journal/JDE/article-full-text-pdf/2262F181060
- Drossner DM, Hirsh DA, Sturm JJ, Mahle WT, Goo DJ, Massey R, et al. Cardiac disease in pediatric patients presenting to a pediatric ED with chest pain. Am J Emerg Med. 2011;29(6):632-638. Available from: https://doi.org/10.1016/j.ajem.2010.01.011
- Bohm P, Barra S, Weizman O, Narayanan K, Meyer T, Schmied C, et al. Sudden cardiac arrest during sports in children and adolescents. Circulation. 2024;149(10):794-796. Available from: https://doi.org/10.1161/circulationaha.123.064739
- Ahmed S, Foulkes L, Leung JT, Griffin C, Sakhardande A, Bennett M, et al. Susceptibility to prosocial and antisocial influence in adolescence. J Adolesc. 2020;84:56-68. Available from: https://doi.org/10.1016/j.adolescence.2020.07.012
- Woodward LJ, Fergusson DM. Life course outcomes of young people with anxiety disorders in adolescence. J Am Acad Child Adolesc Psychiatry. 2001;40(9):1086-1093. Available from: https://doi.org/10.1097/00004583-200109000-00018
- McElhaney KB, Antonishak J, Allen JP. 'They like me, they like me not': popularity and adolescents' perceptions of acceptance predicting social functioning over time. Child Dev. 2008;79(3):720-731. Available from: https://doi.org/10.1111/j.1467-8624.2008.01153.x
- Moideen Sheriff S, Singh G, Chukwunyelu NK, Ezeafulukwe CJ, Hassan OA. Hyperthyroidism masquerading as an anxiety disorder: A report on a misdiagnosed case. Cureus. 2023;15(8):e44071. Available from: https://doi.org/10.7759/cureus.44071
- Niedziela M. Hyperthyroidism in adolescents. Endocr Connect. 2021;10(11):R279-R292. Available from: https://doi.org/10.1530/ec-21-0191
- Zuhur SS, Bilen O, Aggul H, Topcu B, Celikkol A, Elbuken G. The association of TSH-receptor antibody with the clinical and laboratory parameters in patients with newly diagnosed Graves' hyperthyroidism: Experience from a tertiary referral center including a large number of patients with TSH-receptor antibody-negative patients with Graves' hyperthyroidism. Endokrynologia Polska. 2021;72(1):14-21. Available from: https://doi.org/10.5603/ep.a2020.0062
- Scatti Regàs A, Pujol Borrell R, Ferrer Costa R, Puerto Carranza E, Clemente León M. Graves disease with negative TSH receptor antibodies: A presentation of 5 cases. Anales de Pediatría (English Edition). 2020;93:417-419. Available from: https://doi.org/10.1016/j.anpedi.2020.01.008
- Nishihara E, Fukata S, Hishinuma A, Amino N, Miyauchi A. Prevalence of thyrotropin receptor germline mutations and clinical courses in 89 hyperthyroid patients with diffuse goiter and negative anti-thyrotropin receptor antibodies. Thyroid. 2014;24(5):789-795. Available from: https://doi.org/10.1089/thy.2013.0431
- Kleinau G, Vassart G. TSH receptor mutations and diseases. [Updated 2017 Jul 24]. In: Feingold KR, Anawalt B, Blackman MR, et al., editors. Endotext [Internet]. South Dartmouth (MA): MDText.com, Inc.; 2000-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK279140/
- Lemaine V, Cayci C, Simmons PS, Petty P. Gynecomastia in adolescent males. Semin Plast Surg. 2013;27(1):56-61. Available from: https://doi.org/10.1055/s-0033-1347166
Article Alerts
Subscribe to our articles alerts and stay tuned.
 This work is licensed under a Creative Commons Attribution 4.0 International License.
This work is licensed under a Creative Commons Attribution 4.0 International License.

 Save to Mendeley
Save to Mendeley
