Archives of Clinical Gastroenterology
Portal vein septic thrombosis secondary to complicated appendicitis: Case report
Jacqueline Vasconcelos Quaresma1*, Igor Mizael da Costa Saadi2, Rafael José Romero Garcia3 and Leanne Isadora Vasconcelos Quaresma4
2Jean Bitar Hospital, Clinica Médica, Belém, Pará, Brazil
3Santa Casa de Misericórdia of Pará Foundation, Gastrointestinal Surgery, Belém, Pará, Brazil 4Federal University of Pará, Medicine, Belém, Pará, Brazil
Cite this as
Quaresma JV, da Costa Saadi IM, Romero Garcia RJ, Vasconcelos Quaresma LI (2018) Portal vein septic thrombosis secondary to complicated appendicitis: Case report. Arch Clin Gastroenterol 4(2): 023-025. DOI: 10.17352/2455-2283.000053Background: Portal vein septic thrombophlebitis is a rare and serious event of late diagnosis and secondary to intra-abdominal infection.
Case report: A 21-year-old man was admitted to the hospital with loss of weight, fever, chills, hepatosplenomegaly, and history of abdominal pain in the right iliac fossa previously treated with ciprofloxacin. At the entrance physical examination, he was emaciated and had no signs of abdominal pain upon palpation. Computed tomography showed portal vein thrombosis and nodular image in the ileocecal region, initiating antibiotic therapy. After exploratory laparotomy, appendicitis was confirmed and hepatic collections were found. After ten days of the procedure and the end of the antibiotic therapy, he was discharged, keeping well and without complaints.
Conclusions: Septic thrombophlebitis is a rare but serious complication of non-specific signs and symptoms, making diagnosis difficult. Imaging tests are necessary that show the thrombosis to close diagnosis. Treatment should be started early, with the introduction of antibiotics and eradication of the septic focus.
Introduction
Septic thrombosis of the portal vein or pylephlebitis is a rare and serious event, secondary to some infectious intra-abdominal condition that usually includes acute appendicitis, cholangitis, diverticulitis and, less frequently, pancreatitis [1].
The diagnosis is often late because of low clinical suspicion and unspecific symptomatology including fever, abdominal pain, nausea and vomiting. Consequently, complications such as intestinal necrosis, hepatic abscesses and septic shock are common [2].
The diagnosis requires a known abdominal focus of infection and image examination showing portal vein thrombosis. Laboratory tests may show infection and liver dysfunction; cultures usually show gram-negative microorganisms (Bacteroides fragilis, Escherichia coli, Proteus mirabilis, Klebsiella pneumoniae, and enterobacteria species) (Figure 1) [2].
Pylephlebitis can affect individuals in any age group. It is difficult to estimate the incidence of the disease, but a retrospective study of 141 patients indicated a significant increase in the number of cases of septic thrombosis of the portal vein in the last 15-20 years. This fact seems to be related to the advances and greater availability of imaging tests. Mortality was high in the pre-antibiotic era, when it approached 100% [3].
Once the diagnosis is confirmed, the cause must be treated, and antimicrobials should be started without delay. Anticoagulant therapy is still controversial [1].
In this study, we intend to present the case of a patient with septic thrombosis of the portal vein secondary to appendicitis, who underwent exploratory laparotomy with appendectomy and treatment with intravenous antibiotics and responded to the therapy satisfactorily.
Case Report
A 21-year-old male patient from Pará sought emergency medical attention several times with complaints of nausea, vomiting, fever and abdominal pain in the right iliac fossa, which later became diffuse and mild. Treatment with Ciprofloxacin was prescribed for 10 days and there was partial improvement of the pain. However, after the antibiotic treatment was suspended, the patient developed a 6kg weight loss, followed by fever, chills and hepatosplenomegaly, at which point he was admitted to Jean Bitar Hospital 25 days after the symptoms started.
The patient had no previous history of diseases, allergies or surgeries. At the entrance physical examination, he was emaciated, pale, febrile, tachycardic, and icteric (2+ /4+). In cardiac auscultation there was systolic murmur 2+/- 4, and in the pulmonary auscultation the vesicular murmur was reduced in the left pulmonary base. The abdomen was distended, tense, painless to superficial palpation and painful to deep palpation in the right iliac fossa. There was hepatomegaly (3 cm from the costal border) and splenomegaly (6 cm from the costal border).
The hemogram showed severe anemia, leukocytosis with neutrophilia, a significant increase in erythrocyte sedimentation rate and e C-reactive protein. There was alteration of the liver enzymes, mainly an increase of the canalicular ones, as well as an increase of bilirubin at the expense of direct fraction.
The results of blood culture and serologies for toxoplasmosis, leptospirosis, malaria, Chagas disease and leishmaniasis were negative. Upper gastrointestinal endoscopy showed medium and small caliber esophageal varices in the distal third of the esophagus.
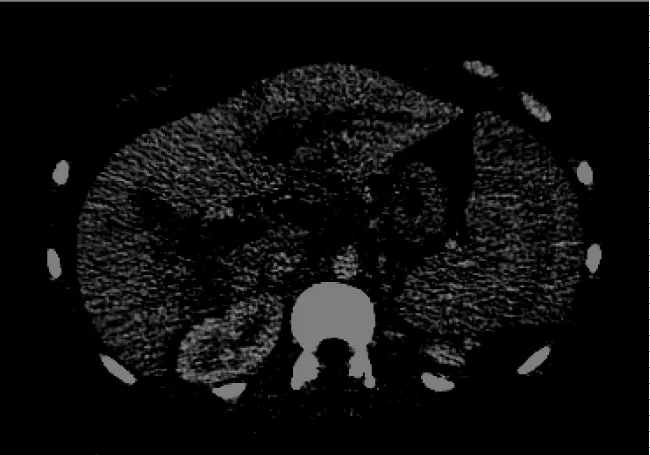
A Computed tomography of the abdomen was performed, showing a large volume ascites, enlarged liver presenting nodular hypovascular images, predominating in the vascular trajectories measuring up to 3.0 cm, portal vein thrombosis with cavernous transformation, enlarged spleen, nodular image of lobulated contours located in the ileocecal region, small volume bilateral pleural effusion. Treatment with a 4th generation cephalosporin associated with metronidazole was initiated. After 14 days, the prescribed antibiotics were discontinued and Piperacillin/Tazobactam was introduced for 10 days (Figure 2).
The patient underwent exploratory laparotomy where a collection in ileocecal location and multiple hepatic collections were observed. He was then submitted to appendectomy, lymph node biopsy and drainage of the abdominal cavity. A histopathological study of the cecal appendix and mesenteric lymph node was done, which showed acute gangrenous appendicitis and chronic reactional lymphadenitis (Figure 3).
The patient recovered with progressive clinical improvement and the drains were removed five days after the surgery. After ten days of the procedure and the end of the antibiotic therapy, he was discharged for outpatient follow-up for esophageal variceal surveillance and remained well and without complaints.
Discussion
Septic thrombophlebitis of the portal vein or its tributaries is characterized by an uncommon and severe complication of suppurative infections in regions drained by the portal vein, with diverticulitis and appendicitis being the most frequent causes, and may also be caused by cholangitis, pelvic infections and, less often, pancreatitis [1,4].
The incidence of pylephlebitis secondary to appendicitis was reduced due to modern antibiotic therapy and surgical treatment of appendicitis. However, the mortality of this complication occurs in 30% to 50% of the cases [1,5]. These numbers are a consequence of the normally late diagnosis due to the absence of specific symptoms [1,3]
The pathogenesis is not well known; therefore, two mechanisms are proposed. The first one would be a bacterial translocation and adhesion of the infectious agent to the endothelium, which in turn triggers the coagulation cascade and thrombus formation. The second one would be the occurrence of thrombosis, in an already predisposed environment, followed by infection [6].
The most commonly described symptoms are abdominal pain, fever, nausea, vomiting, diarrhea, weight loss, and less often, jaundice. Hepatomegaly is rarely found and is mainly observed in subacute cases of the disease [2]. At admission, this patient’s case syndromically presented itself as febrile hepatosplenomegaly and the diagnostic investigation was oriented in this spectrum of diseases. However, due to the twenty-five days period, we were faced with the complication of septic thrombosis.
The diagnosis is made by imaging tests, being the Doppler ultrasonography and the tomography the most used ones. However, computed tomography (CT) is described by some authors as the most sensitive in the identification of thrombi in the mesenteric veins and visualization of hepatic abscesses [7]. Corroborating with the literature, the elucidative test in this case was the tomography of the abdomen.
In laboratory tests, left shift leukocytosis, alkaline phosphatase increase, and hepatic dysfunction are common [2,3]. Bacterial growth in blood culture usually occurs in 80% of patients with pylephlebitis. The main bacteria found are from the intestinal flora of the patient, being Bacterioides fragilis and Escherichia coli the most frequent cause of septic thrombi. It is not necessary to wait for the result of the blood culture to start treatment [1,3].
The conservative treatment of pylephlebitis with the use of broad-spectrum antibiotics for at least six weeks along with the surgical elimination of the septic focus have had excellent results and decreased mortality rates [2,4]. The use of anticoagulation is controversial in these cases, without studies demonstrating significant benefits to the patient. However, some authors point out the use of anticoagulant for at least six months, especially in environments with hypercoagulation or with risk factors for this scenario [4].
In this case, the anticoagulant was not used because it was still a questionable procedure; moreover, because it was a late diagnosis, and the patient already had a cavernous transformation of the portal vein, the medication was no longer a modifier of the disease.
It is important to start treatment as soon as possible since its delay can result in unfavorable outcomes such as multiple hepatic abscesses; complications due to portal hypertension, such as esophageal varices and splenomegaly; or mesenteric ischemia [5,4].
Conclusion
Septic thrombosis of the portal vein and its tributaries is a rare and serious event, secondary to suppurative infections of the abdomen. Its diagnosis requires imaging tests, such as Doppler ultrasonography and computed tomography, to be established. Treatment consists of a combination of broad spectrum antibiotics and the eradication of the septic focus, usually through surgery. What is important in these cases is to initiate treatment as soon as possible to avoid more serious complications and to increase patient survival.
- Tang R (2015) Intestinal infarction caused by thombophlebitis of the portomesenteric veins as a complication of acute grangrenous appendicitis after appendectomy. A case report. Medicine. 94: Link: https://goo.gl/LxMhck
- Garrett A (2014) Once universally fatal:pylephlebitis. The american journal of medicine. 127: Link: https://goo.gl/btfSvk
- Fonseca-Neto OCL, Vieira LPF, Miranda AL (2007) Tromboflebite séptica da veia porta secundária a apendicite. Arq Bras Cir Dig. 20:137-8. Link: https://goo.gl/A7sYNi
- Mariam A, Guillermo B, Pilar N, Belén B, Grueso L, et al. (2007) Septic thrombophlebitis of the superior mesenteric vein and liver abscesses in a patient with Crohn's disease. BMC gastroenterology. 22: DOI: 10.1186/1471-230X-7-22. Link: https://goo.gl/RrrXjn
- Grabala M, Grabala P, Malinowski P, Adadyński L (2017) Superior mesenteric and portal vein thrombosis following appendectomy – A case report. Polish Annals of Medicine. 24: 55-59. ISSN 1230-8013. Link: https://goo.gl/saMJd5
- Roberto AG, Daniela MS, Barros, Maria da Gloria CRM, Marcelo AV, et al. (2010) Pileflebite mesentérica secundária à diverticulite - Mesenteric pylephlebitis secondary a diverticulitis. GED gastroenterol. endosc. dig; 29: Link: https://goo.gl/NDvTnf
- Carnish MD (2015) A case of septic portal vein thrombosis (pylephlebitis). In: The Medicine Forum. p21. Link: https://goo.gl/QzB3Hd
Article Alerts
Subscribe to our articles alerts and stay tuned.
 This work is licensed under a Creative Commons Attribution 4.0 International License.
This work is licensed under a Creative Commons Attribution 4.0 International License.



 Save to Mendeley
Save to Mendeley
