Archives of Clinical Gastroenterology
Percutaneous choledocho-duodenal shunt for malignant biliary obstruction
Saburo Kakizoe*, Yumiko Kakizoe, Hiroshi Kakizoe and Keiji Kakizoe
Cite this as
Kakizoe S, Kakizoe Y, Kakizoe H, Kakizoe K (2018) Percutaneous choledocho-duodenal shunt for malignant biliary obstruction. Arch Clin Gastroenterol 4(1): 018-019. DOI: 10.17352/2455-2283.000051We developed a new method: percutaneous choledocho-duodenal shunt (PCDS) for complete biliary obstruction patient. At first, percutaneous transhepatic cholangio drainage (PTCD) is performed as usual manner with local anesthesia. After the patient is recovered from bilirubinemia, percutaneous endoscopic gastrostomy (PEG) is performed with pull-through method under local anesthesia. Catheter of PEG is replaced to jejunal catheter after the gastrostomy is completed. These two catheters (catheter of PTCD and Jejunal catheter) are connected each other with extra-peritoneal shunt. The method is useful for the patient with complete biliary obstruction who cannot be performed biliary stenting.
Introduction
The self-expandable metallic stent has been a standard procedure for the patient with malignant biliary obstruction [1-3]. However the procedure cannot be performed for the patient with complete biliary obstruction which rejects guide wire insertion before stenting. We design the new procedure; Percutaneous Choledocho-Duodenal Shunt (PCDS) for a patient with such a complete biliary obstruction.
Methods
At first, percutaneous transhepatic cholangio drainage (PTCD) is performed as usual manner with local anesthesia. After the patient is recovered from bilirubinemia, percutaneous endoscopic gastrostomy (PEG) is performed with pull-through method under local anesthesia [4]. Catheter of PEG is replaced to jejunal catheter after the gastrostomy is completed. After we replace PTCD catheter to 12F catheter (Create Medic. Japan), these two catheters (catheter of PTCD and Jejunal catheter) are connected each other with making extra-peritoneal shunt (Figure 1a,b).
Results
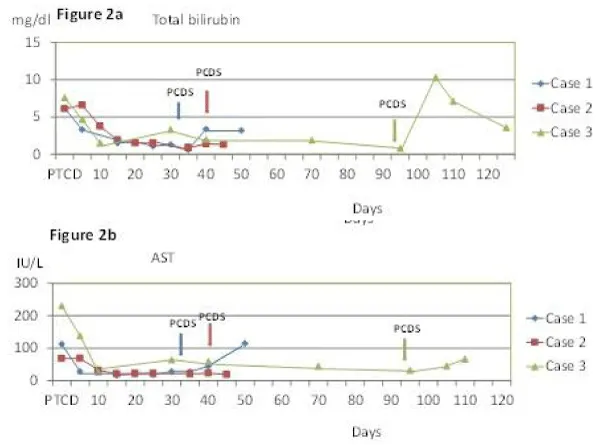
After adequate informed consent, we performed the procedure for three patient since July 11th 2013. First case was 92 year old female who suffered pancreatic head cancer with multiple liver and lung metastasis. Total bilirubin and other serum data like AST decreased after PTCD and kept normal range after PCDS until she had multiple hepatic metastasis and peritonitis carcinomatosa (Figure 2a,b). She could take bath and enjoy her life until she died with cancer 34 days after PCDS. Second case was 87 year old male who suffered cholangiocarcinoma. His bile duct stent was obstructed by enlarged cancer. PCDS was performed without any trouble and he died with peritonitis carcinomatosa 10 days after PCDS. The third case was 83 year old male who suffered pancreatic head cancer with retroperitoneal invasion. Because he had severe heart failure, he could not be performed surgery with general anesthesia. PCDS was performed without complication. He could take bath and enjoy his life for 50days after PCDS and died with cancer.
Discussion
Although the self-expandable metallic stents have been a standard procedure for the patient with unresectable malignant biliary and/or pancreatic head cancer, a few patients cannot be performed because of complete obstruction of their common bile duct [5]. In addition, some serious complications such as acute pancreatitis or acute cholecystitis were reported after self-expandable metallic biliary stent [1,3,6]. For those patients we consider the choledocho-jejunostomy with open or laparoscopic approach. However the procedure is too invasive to perform for some aged patients and/or end-stage cancer patients. Therefor usually those patients live with PTCD catheter for their terminal period. PCDS is easy to perform by ordinary gastroenterologist with relatively low cost. PCDS may bring a little happiness for those patients with minimal invasive procedures [5,7].
Long term prognosis is unknown because these cases were died with cancer only a month after PCDS. In my opinion, one-way shunt valve may be useful to keep the shunt flow for long term. A multicenter randomized controlled trial is required to confirm the benefits of PCDS.
- Kitano M, Yamashita Y, Tanaka K, Konishi H, Yazumi S, et al. (2013) Covered self-expandable metal stents with an anti-migration system improve patency duration without increased complications compared with uncovered stents for distal biliary obstruction caused by pancreatic carcinoma: a randomized multicenter trial. Am J Gastroenterol 108: 1713-1722. Link: https://goo.gl/jCHxYv
- Mosconi C, Renzulli M, Giampalma E, Galuppi A, Balacchi C, et al. (2013) Unresectable perihilar cholangiocarcinoma: multicmodal palliative treatment. Anticancer Res 33: 2747-2753. Link: https://goo.gl/4vKqWR
- Itoi T, Sofuni A, Itokawa F, Tonozuka R, Ishii K (2013) Current status and issues regarding biliary stenting in unresectable biliary obstruction. Dig Endosc 2: 63-70. Link: https://goo.gl/fdQEaD
- Grant JP (1993) Percutaneous endoscopic gastrostomy; initial placement by single endoscopic technique and long-term follow-up. Ann Surg 217: 168-174. Link: https://goo.gl/mqUEai
- Park DH, Jeong SU, Lee BU, Lee SS, Seo DW, et al. (2013) Prospective evaluation of a treatment algorithm with enhanced guidewire manipulation protocol for EUS-guided biliary drainage after failed ERCP. Gastrointest Endosc 78: 91-101. Link: https://goo.gl/w9tDhc
- Hyun D, Park KB, Hwang JC, Shin BS (2013) Delayed, life-threatening hemorrhage after self-expandable metallic biliary stent placement: clinical manifestations and endovascular treatment. Acta Radiol 54: 939-943. Link: https://goo.gl/RHC3cR
- Ljungdahl M, Sundbom M (2006) Complication rate lower after percutaneous endoscopic gastrostomy than after surgical gastrostomy: a prospective, randomized trial. Surg Endosc 20: 1248-1251. Link: https://goo.gl/ThbT3K

Article Alerts
Subscribe to our articles alerts and stay tuned.
 This work is licensed under a Creative Commons Attribution 4.0 International License.
This work is licensed under a Creative Commons Attribution 4.0 International License.

 Save to Mendeley
Save to Mendeley
