Case Report of a Broken Tip of a Thrombus Aspiration Catheter in an Acute Coronary Syndrome in a Patient with Heart Block
MD Cardiology, FSCAI, Head of cath lab of Nabdh Al- Hayat Cardiac Center, Mukalla, Hadhramout Gov., Yemen
Author and article information
Cite this as
Bafadhl TA. Case Report of a Broken Tip of a Thrombus Aspiration Catheter in an Acute Coronary Syndrome in a Patient with Heart Block. Open J Trauma. 2026; 10(1): 001-004. Available from: 10.17352/ojt.000052
Copyright License
© 2026 Bafadhl TA. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.We describe 67 years old male patient presenting with acute coronary syndrome (acute inferior ST elevation) with complete heart block. Primary percutaneous coronary intervention was decided with temporary pacemaker insertion. In view thrombus burden lesion in the proximal right coronary artery. We did thrombus aspiration using a thrombus aspiration catheter. After successfully aspirating thrombus, resistance was felt on withdrawal of the aspiration catheter. The tip of the thrombus aspiration catheter was broken and retained in the guide wire at the level of the proximal right coronary artery. The broken tip of the thrombus aspiration catheter was successfully retrieved percutaneously.
In ST elevation myocardial infarction (STEMI), percutaneous coronary intervention is superior to thrombolysis in terms of in-hospital mortality, reinfarction, and stroke [1]. Coronary atherosclerotic plaque rupture with thrombus formation being the basic pathophysiologic phenomenon in acute myocardial infarction, prevalence of thrombus is commonly seen in STEMI compared to non-ST elevation myocardial infarction (NSTEMI) [2].
Thrombus aspiration in patients with high thrombus burden can decrease thrombus burden, lower rates of distal embolization, improve thrombolysis in myocardial infarction- 3 flow, reduce the incidence of no reflow, improve microvascular perfusion, and consequently improve clinical outcomes. However, >2 dozen randomized trials have compared the outcomes of routine thrombus aspiration with primary percutaneous coronary intervention (PCI) alone in patients with ST- segment– elevation myocardial infarction (STEMI) and have not shown a consistent reduction in cardiovascular outcomes. As such, routine thrombus aspiration during primary PCI is not recommended by guideline committees (class III, 2021 American College of Cardiology/American Heart Association guidelines or 2017 European Society of Cardiology guidelines) [3,4].
Case report
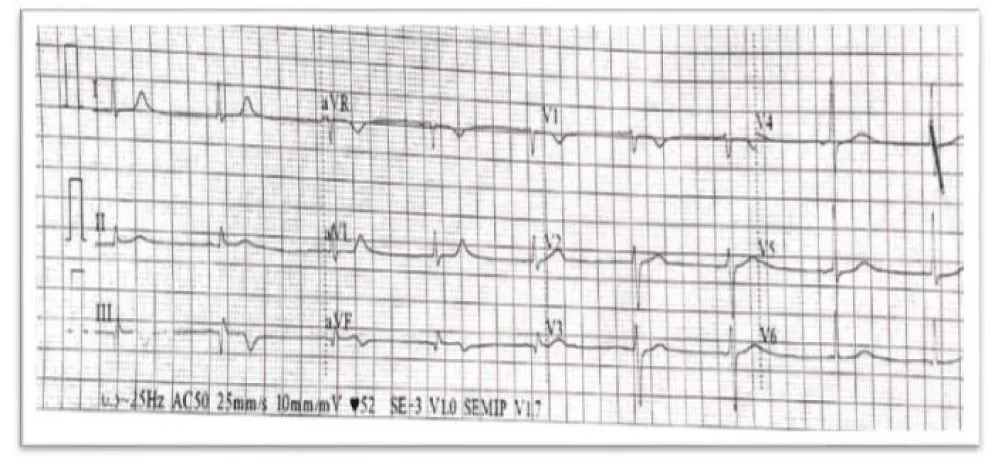
A male patient aged 67 years old with a history of diabetes Mellitus type II (DM), presented to the emergency department of a private hospital with central chest pain increasing in intensity 3 hours before arrival, with a history of sweating and nausea. ECG done on arrival (Figure 1).
The patient was subsequently admitted to the intensive care unit (ICU). On arrival, vital signs were as follows: blood pressure 90/60 mmHg, heart rate 60 beats/min, and temperature 37 °C. Physical examination revealed no pallor or jaundice, no lower-limb edema, and intact peripheral pulses. Abdominal examination showed no organomegaly. Chest examination was unremarkable with normal breath sounds. Cardiac examination demonstrated normal first and second heart sounds with no added sounds or murmurs.
Because the patient’s chest pain had decreased in intensity, thrombolytic therapy was unfortunately not administered. In addition, the admitting hospital lacked percutaneous coronary intervention (PCI) capability. Consequently, conservative management was initiated, including antiplatelet therapy, anticoagulation, and statin therapy. The patient remained in the ICU for one day.
On the following day, the patient developed dizziness and recurrent episodes of shortness of breath. He requested expert consultation and was transferred to Nabdh Al-Hayat Cardiac Center (NCC) in Mukalla for further evaluation and management.
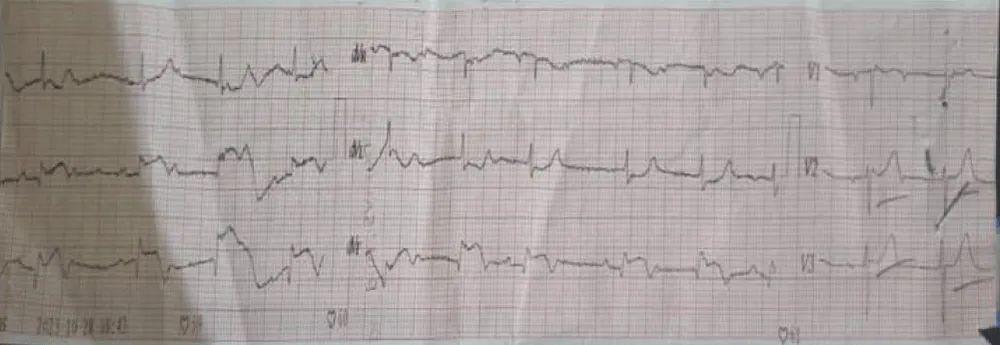
At NCC, reassessment revealed significant hemodynamic deterioration. Vital signs were as follows: blood pressure 80/50 mmHg, heart rate 40 beats/min, and temperature 37 °C. Electrocardiography was performed (Figure 2). Bedside transthoracic echocardiography demonstrated normal left-sided cardiac structure with preserved left ventricular systolic function, no resting regional wall-motion abnormalities, and no mitral regurgitation. No mechanical complications were identified, including ventricular septal rupture, free-wall rupture, or papillary muscle dysfunction. However, the right ventricle was dilated with global hypokinesia.
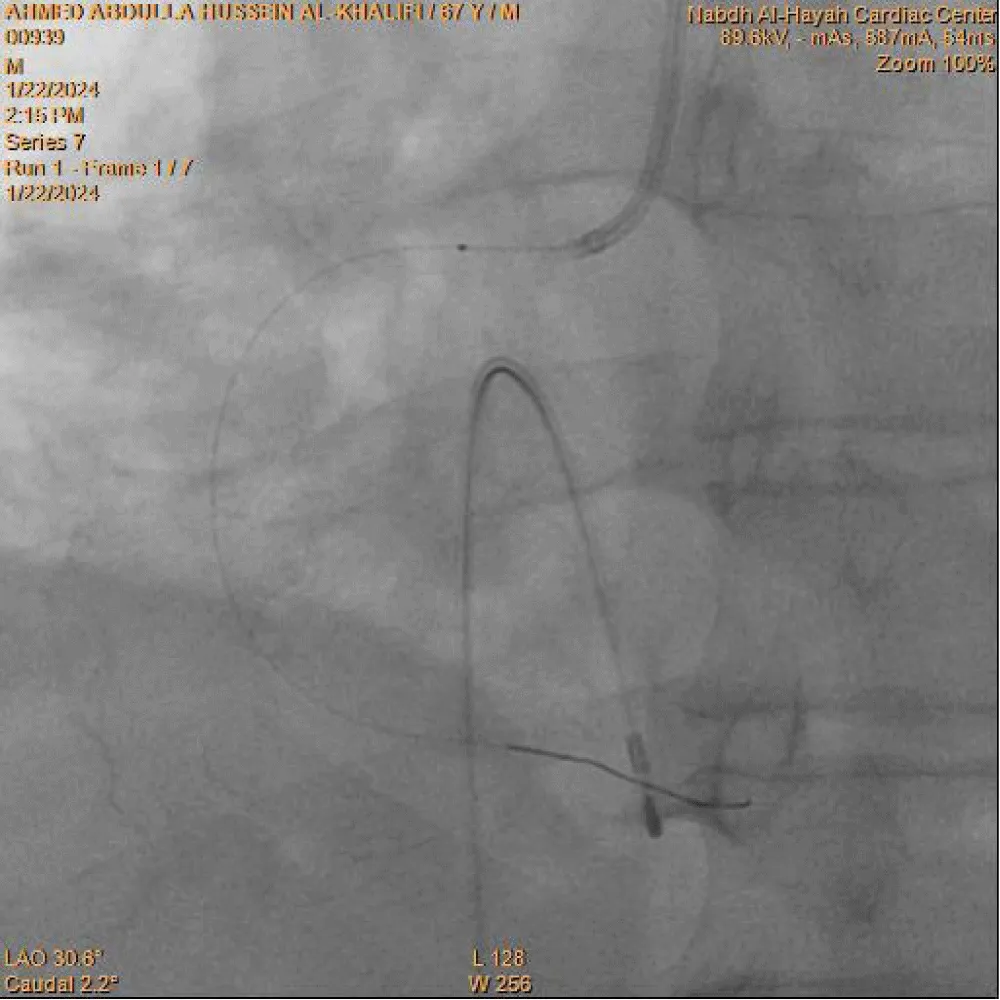
Primary percutaneous coronary intervention (PCI) was decided, and the catheterization laboratory team was immediately activated. A trans-femoral venous approach was used for temporary pacemaker insertion, which was successfully established at a fixed rate of 60 beats/min. An initial attempt at right radial artery puncture for coronary angiography was unsuccessful; therefore, crossover to the right femoral artery was performed.
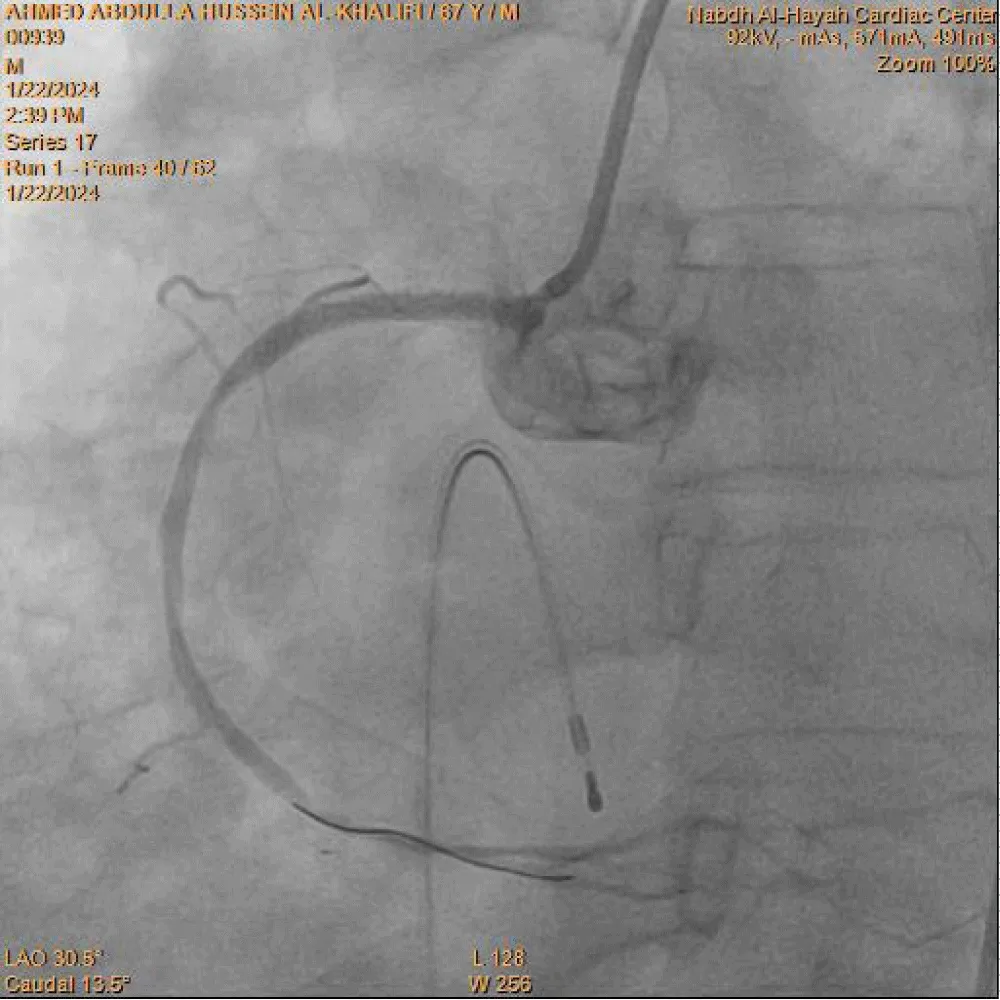
Coronary angiography was carried out using a 6-Fr diagnostic left Judkins catheter, which revealed an atherosclerotic left coronary system. A right Judkins guiding catheter was then used to cannulate the right coronary artery (RCA), demonstrating total occlusion of the proximal RCA with a high thrombus burden. The occluded segment was successfully crossed with a 0.014-inch BMW PTCA floppy guidewire. Limited thrombus aspiration was achieved after five passes using a 6-Fr Export aspiration catheter (Medtronic), as shown in Figure 3. Control angiography of the RCA after thrombus aspiration demonstrated TIMI I flow. Subsequently, a 1.25 × 10 mm Sprinter balloon (Medtronic Inc.) was advanced over the guidewire for balloon predilatation. Upon reaching the proximal RCA, three radiopaque markers were visualized instead of the expected two (Figure 4). This immediately raised suspicion of a device fracture. Careful inspection of the Export catheter, which had just been withdrawn from the guiding catheter and was lying on the table, confirmed loss of its distal tip. This represented a precarious situation, with a thrombogenic broken catheter fragment retained within a thrombus-laden coronary artery and loss of operator control over the fragment.
Given the very short distance between the distal balloon marker and the third radiopaque marker, it was inferred that only the distal tip of the Export catheter had fractured (Figure 5). An attempt to advance a smaller 1.0 × 10 mm Sprinter balloon distal to the retained fragment over the original guidewire was unsuccessful. Therefore, a second BMW PTCA guidewire was advanced into the distal RCA. A 2.0 × 12 mm Sprinter PTCA balloon was then advanced and positioned distal to the fractured catheter tip. The balloon was inflated to 8 atm and gently withdrawn from the mid to proximal RCA, successfully entrapping and retrieving the broken Export catheter tip into the guiding catheter.
The entire system, including the guiding catheter, both BMW PTCA guidewires, the balloon, and the fractured aspiration catheter tip, was removed en bloc. The guiding catheter was flushed with heparinized saline, and the retrieved broken catheter tip was clearly identified. The RCA was subsequently re-engaged using a new JR 3.5 guiding catheter, and a fresh BMW PTCA guidewire successfully crossed the proximal RCA lesion. Predilatation was performed using a 2.0 × 12 mm Sprinter balloon, restoring TIMI III flow. A 3.0 × 30 mm drug-eluting stent was then deployed in the proximal RCA and inflated to 14 atm. Final angiography demonstrated TIMI III flow with good stent expansion and no evidence of edge dissection (Figure 6).
Discussion
The incidence of broken or retained percutaneous coronary intervention (PCI) hardware in earlier literature is approximately 0.2% [5]. Although significant refinement in device design has occurred over the past decade, the increasing number and complexity of percutaneous coronary procedures continue to be associated with occasional intravascular hardware failure. Several reports have described successful retrieval of fractured catheters, guidewires, balloons, and both expanded and unexpanded stents from the intracoronary circulation using various techniques [5-7]. Familiarity with these retrieval methods is essential, as no single technique is universally effective in all clinical scenarios.
Cagdas Akgullu et al. [8] reported a case of a trapped thrombus aspiration catheter in a coronary artery caused by rupture of the main shaft and twisting over the guidewire; the device was successfully removed by withdrawing the entire system. Other case reports have described complications related to thrombus aspiration catheters, including thrombus formation in the left main coronary artery and inadvertent coronary endarterectomy using the Thrombuster III GR catheter [9,10].
A review of 48 case reports involving a total of 67 patients with guidewire entrapment showed that 41.8% were managed by percutaneous extraction, 43.3% required surgical intervention, and 14.9% were treated conservatively. Various percutaneous retrieval techniques have been described, including stenting the fragment against the vessel wall, snare loop capture, double- or triple-wire techniques, use of a bioptome, Tornus microcatheter, deep guide catheter wedging with balloon inflation, and pigtail catheter manipulation [11].
In a prior report assessing the prevalence and outcomes of fractured PCI hardware, 12 out of 5,400 percutaneous transluminal coronary angioplasty (PTCA) procedures were complicated by retained components, including guidewire fragments, balloon catheters, and guide catheters [12]. Follow-up of patients with retained guidewire fragments revealed no clinical sequelae over a period ranging from 6 to 60 months, suggesting that management decisions should be individualized. Not all cases of retained hardware necessitate coronary artery bypass grafting (CABG), particularly when fragments are located in chronically occluded or distal vessels [12]. Additional reports have documented successful retrieval of an FFR wire tip using an angiographic catheter (Slip-Cath) via the mother–child technique [13], as well as balloon-assisted extraction of a fractured Export catheter [14].
Retained intracoronary hardware can act as a nidus for thrombus formation, potentially leading to acute vessel occlusion, myocardial infarction, arrhythmias, coronary perforation, or embolic events [15]. Therefore, removal of the fractured fragment is generally recommended. In our patient, the presence of a thrombogenic milieu with thrombus formation proximal to the broken catheter significantly increased the risk of further thrombus propagation, making prompt retrieval of the fractured Export catheter tip imperative.
Potential causes of retained PCI hardware include excessive torqueing, forceful catheter withdrawal, improper handling, device reuse, manufacturing defects, inadvertent advancement of large-caliber catheters through smaller access sheaths, polymer aging, or a combination of these factors.
Conclusion
This case highlights a rare but serious complication of thrombus aspiration during primary percutaneous coronary intervention. Prompt recognition of catheter fracture and familiarity with percutaneous retrieval techniques enabled successful removal without surgical intervention. Awareness of such device-related complications and preparedness for their management are essential to ensure procedural safety and optimal clinical outcomes.
- Zijlstra F. Angioplasty vs thrombolysis for acute myocardial infarction. Eur Heart J. 2003;24:21–23. Available from: https://doi.org/10.1016/s0195-668x(02)00693-0
- Sianos G, Papafaklis MI, Daemen J, Vaina S, van Mieghem CA, van Domburg RT, et al. Angiographic stent thrombosis after routine use of drug-eluting stents in ST-segment elevation myocardial infarction: the importance of thrombus burden. J Am Coll Cardiol. 2007;50:573–583. Available from: https://doi.org/10.1016/j.jacc.2007.04.059
- Lawton JS, Tamis-Holland JE, Bangalore S, Bates ER, Beckie TM, Bischoff JM, Bittl JA, Cohen MG, DiMaio JM, Don CW, et al. 2021 ACC/AHA/SCAI guideline for coronary artery revascularization: executive summary. Circulation. 2022;145:e4–e17. Available from: https://doi.org/10.1016/j.jacc.2021.09.006
- Agewall S, Antunes MJ, Bucciarelli-Ducci C, Bueno H, Caforio ALP, Crea F, Goudevenos JA, Halvorsen S, et al. 2017 ESC guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Eur Heart J. 2018;39:119–177. Available from: https://doi.org/10.1093/eurheartj/ehx393
- Hartzler GO, Rutherford BD, McConahay DR. Retained percutaneous transluminal coronary angioplasty equipment components and their management. Am J Cardiol. 1987;60(16):1260–1264. Available from: https://doi.org/10.1016/0002-9149(87)90604-7
- Schneider RM, Fornes RE, Stuckey WC, Gilbert RD, Peter RH. Fracture of a polyurethane cardiac catheter in the aortic arch: a complication related to polymer aging. Cathet Cardiovasc Diagn. 1983;9(2):197–207. Available from: https://doi.org/10.1002/ccd.1810090212
- Gurley JC, Booth DC, Hixson C, Smith MD. Removal of retained intracoronary percutaneous transluminal coronary angioplasty equipment by a percutaneous twin guidewire method. Cathet Cardiovasc Diagn. 1990;19(4):251–256. Available from: https://doi.org/10.1002/ccd.1810190408
- Akgullu C, Eryilmaz U, Gungor H, Zencir C, Avcil M, Dagli B. A case of thrombus aspiration catheter trapped in coronary artery due to rupture of its main shaft and twisting over the wire. J Clin Exp Cardiol. 2014;5:5. Available from: https://www.longdom.org/open-access/a-case-of-thrombus-aspiration-catheter-trapped-in-coronary-artery-due-to-rupture-of-its-main-shaft-and-twisting-over-the-49392.html
- Alazzoni A, Velianou J, Jolly SS. Left main thrombus as a complication of thrombectomy during primary percutaneous coronary intervention. J Invasive Cardiol. 2011;23:E9–E11. Available from: https://pubmed.ncbi.nlm.nih.gov/21297218/
- Taguchi E, Sakamoto T, Kamio T, Kotono Y, Suzuyama H, Fukunaga T, et al. Inadvertent coronary endarterectomy during aspiration thrombectomy with a Thrombuster III GR catheter in a patient with acute coronary syndrome. Cardiovasc Interv Ther. 2013;28:222–225. Available from: https://doi.org/10.1007/s12928-012-0151-y
- Al-Moghairi AM, Al-Amri HS. Management of retained intervention guide-wire: a literature review. Curr Cardiol Rev. 2013;9:260–266. Available from: https://doi.org/10.2174/1573403x11309030010
- Hartzler GO, Rutherford BD, McConahay DR. Retained percutaneous transluminal coronary angioplasty equipment components and their management. Am J Cardiol. 1987;60:1260–1264. Available from: https://doi.org/10.1016/0002-9149(87)90604-7
- Prakash S, Mahla H, Bhairappa S, Somanna S, Manjunath C. Successful retrieval of fractured pressure wire tip (FFR) by hybrid technique. J Saudi Heart Assoc. 2015;27:118–122. Available from: https://doi.org/10.1016/j.jsha.2014.09.001
- Mehta V, Pandit BN, Trehan V. Retrieval of broken export catheter during primary angioplasty. Int J Angiol. 2013;22:185–188. Available from: https://doi.org/10.1055/s-0033-1347897
- Hong YM, Lee SR. A case of guide wire fracture with remnant filaments in the left anterior descending coronary artery and aorta. Korean Circ J. 2010;40(9):475–477. Available from: https://doi.org/10.4070/kcj.2010.40.9.475
Article Alerts
Subscribe to our articles alerts and stay tuned.
 This work is licensed under a Creative Commons Attribution 4.0 International License.
This work is licensed under a Creative Commons Attribution 4.0 International License.



 Save to Mendeley
Save to Mendeley
