Open Journal of Trauma
Perfusion Computed Tomography at Posttraumatic Cerebral Fat Embolism
Alex Trofimov*, George Kalentyev, Michail Yuryev, Alevtina Ruzavina, Kristina Ksenofontova and Michael Karelsky
Cite this as
Trofimov A, Kalentyev G, Yuryev M, Ruzavina A, Ksenofontova K, et al. (2017) Perfusion Computed Tomography at Posttraumatic Cerebral Fat Embolism. Open J Trauma 1(2): 029-031. DOI: 10.17352/ojt.000007The article reports a clinical case illustrating favorable outcome of nonsurgical treatment of a polytraumazed patient with occult severe cerebral fat embolism. The peculiar characteristics of the perfusion CT are demonstrated.
Introduction
Cerebral fat embolism (СFE) is one of the gravest complications in an acute posttraumatic period. According to data obtained by different authors its frequency in severe injuries varies from 0.5% to 30%. Its development is most often caused by fractures of the pelvis, long bones, by massive damage of subcutaneous fat [1].
Despite diverse suggested methods of treatment the mortality in case of the СFE development reaches nearly 70% [2].
In this connection, the possibility for the early FE diagnosing is of particular importance [1]. However, the role of radiological methods still remains to this day quite limited [3].
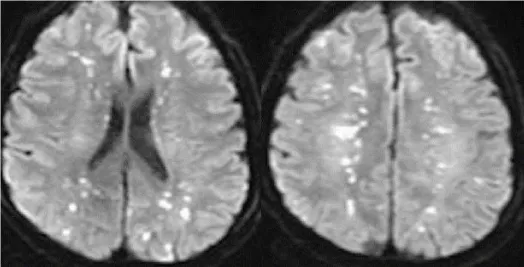
The use of magnetic resonance imaging (MRI) in patients with clinically diagnosed СFE has enabled to describe the so-called “starfield pattern”, which is evident as multiple minor hyperintense foci of cortical-subcortical localization identified in the diffusion-weighted image (DWI) mode [3].
The emergence of such a pattern was explained with the development of a cytotoxic edema in the area of the blood supply to the terminal branches of the cerebral arteries affected by fat emboli [4] (Figure 1).
The MRI semiotics was further exacted [5,6]. It was noted that at the subacute CFE stage on T2-weighted images some hyperintense foci may be identified in the gray and white matter corresponding to vasogenic edema loci around an area of embolism [7].
Furthermore, when using gradient-echo sequences (T2*-GE, SWI, SWAN, etc.) in FE patients petechial hemorrhages may be visualized in perivascular spaces [8].
However, in case of severe injuries patients oftentimes may not be subjected to MRI because of available metal implants and external apparatus for osteosynthesis (f.e., Ilizarov’s apparatus) made of ferromagnetic materials [5].
But the use of the native computer tomography in case of CFE is limited because of its low diagnostic value [3].
On the another hand, the emergence and widespread routine-practice implementation of modern contrast methods for the cerebral microcirculation assessment, such as the perfusion computer tomography (PCT), may significantly improve the CFE diagnosing and promptly start the expert care thereof [7].
Case Summary
A 36-years-old White male without past medical history was admitted with polytrauma after a road traffic accident to the Nizhny Novgorod Regional Trauma Center Level 1 on 22nd January, 2015. There was no clinical evidence of any traumatic brain injury. Initial CT scanning of the whole body and brain revealed no brain damage.
On 23th January 2015 the surgery was performed including an osteosynthesis of the left femur and tibia by Ilizarov’ s apparatus.
Although the treatment performed the development of the twilight disorder of consciousness, uncriticality and respiratory distress were noted on 23rd January 2015. A venous blood test showed multiple fat globules. The development of cerebral and pulmonary fat embolism was diagnosed.
The further venous blood re-tests (24 and 25 January 2015) revealed no fat globules.
However, despite the performed therapy the following clinical evidence of CFE still remained: diplopia and agitation, paresis of VII, VIII and XII cranial nerves.
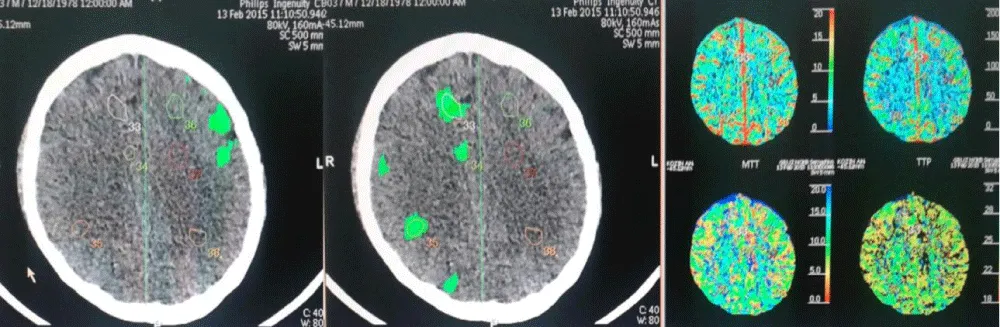
To assess the cerebral microcirculation state, a perfusion brain CT was performed (Figure 2).
The said cerebral perfusion changes were assessed by two independent radiologists as multiple foci of acute ischemic brain damage. The suggestion was made on the continuing CFE.
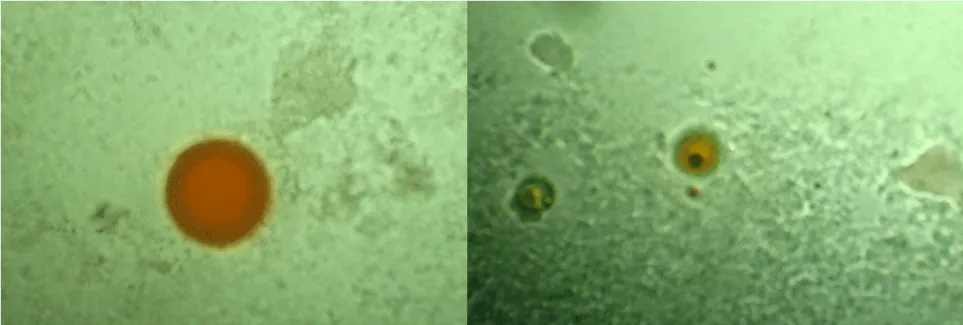
To make diagnosis, blood samples were drawn both from a vein and from a femoral artery. The findings showed no fat globule in venous samples but large globules available in arterial blood (Figure 3).
Thus, there was identified the acute hypoxic encephalopathy secondary to cerebral vessel fat embolism.
A specialized respiratory therapy was started (normobaric hyperoxia at the oxygen flow of 3.5 l/min under the cerebral oxymetry control). As recommended the hypolipidemic therapy with atorvastatin was assigned as well as anticoagulant and disaggregant therapy [1].
During the next few days the patient’s condition significantly improved as follows: focal symptoms regressed, psychotic phenomena stopped, the consciousness recovered to its normal state.
The patient was discharged in a satisfactory condition upon the expiry of 50 days after the injury for the follow-up step-wise care with using an Ilizarov’ s apparatus for osteosynthesis with the satisfactory comparison of bone fragments.
Discussion
Cerebral fat embolism is a dangerous life-threatening complication of an acute period in fractures of long bones and pelvis. It most often causes the simultaneous brain damage and pulmonary injury [9,10].
However, the aspects of using neuroimaging for CFE diagnosis still remain poorly studied [11].
We have carried out the clinical observation of a patient with a prolonged and atypical CFE course and a concurrent severe concomitant injury, wherein the use of current methods for assessing the cerebral microcirculation have enabled to timely identify and arrest its manifestation.
It should be noted that CFE are, in fact, cumulative small-focal cerebral infarctions in the aftermath of embolism of terminal branches of the brain arteries by fat globules [11].
From these positions there become apparent both the mechanism of MR «starfield pattern» phenomenon and the similar pattern of cerebral microcirculation disorders obtained by us with the aid of PCT [11,12].
From the practical point of view the use of the PCT method for diagnosing CFE is affordable for performance at any trauma center and may considerably improve its timely diagnosis and the start of appropriate treatment.
It should be herewith noted that the use of any contrast-enhanced CT techniques in patients with severe extracranial injuries is only possible after the thorough assessment of the risk of nephropathy development and that requires the further deep study and the elaboration of this problem.
- Gupta B, D’souza N, Sawhney C, Farooque K, Kumar A, et al. (2011) Analyzing fat embolism syndrome in trauma patients at AIIMS Apex Trauma Center, New Delhi, India. J Emerg Trauma Shock 4: 337-341. Link: https://goo.gl/ocBybY
- Volgas D, Burch T, Stannard JP, Ellis T, Bilotta J, et al. (2010) Fat embolus in femur fractures: a comparison of two reaming systems. Injury 41: S90-S93. Link: https://goo.gl/JM5HDw
- Parizel P, Demey H, Veeckmans G, Verstreken F, Cras P, et al. (2001) Early diagnosis of cerebral fat embolism syndrome by diffusion-weighted MRI (starfield pattern). Stroke 32: 2942-2944. Link: https://goo.gl/V0DFMB
- Butteriss D, Mahad D, Soh C, Walls T, Weir D, et al. (2006) Reversible cytotoxic cerebral edema in cerebral fat embolism. Am J Neuroradiol 27: 620-623. Link: https://goo.gl/8EFUJ3
- Makarewich СA, Dwyer KW, Cantu RV (2015) Severe Neurologic Manifestations of Fat Embolism Syndrome in a Polytrauma Patient. Am J Orthop 1: 25-28. Link: https://goo.gl/QBuBzR
- Kuo KH, Pan YJ, Lai YJ, Cheung WK, Chang FC, et al. (2014) Dynamic MR Imaging Patterns of Cerebral Fat Embolism: A Systematic Review with Illustrative Cases. Am J Neuroradiol 35: 1052-1057. Link: https://goo.gl/xSSVqB
- Kumar S, Gupta V, Aggarwal S, Singh P, Khandelwal N (2012) Fat embolism syndrome mimicker of diffuse axonal injury on magnetic resonance imaging. Neurol India 60: 100-102. Link: https://goo.gl/rrQgR3
- Zaitsu Y, Terae S, Kudo K, Tha KK, Hayakawa M, et al. (2010) Susceptibility-weighted imaging of cerebral fat embolism. J Comput Assist Tomogr 34: 107-112. Link: https://goo.gl/BlfZZs
- Chrysikopoulos H, Maniatis V, Pappas J, Filalithis P, Gogali C, et al. (1996) Case Report: Post-Traumatic Cerebral Fat Embolism: CT and MR findings. Report of Two Cases and Review of the Literature. Clin Radiol 10: 728-732. Link: https://goo.gl/D0KtJs
- Pape HC, Tornetta P, Tarkin I, Tzioupis C, Sabeson V, et al. (2009) Timing of fracture fixation in multitrauma patients: the role of early total care and damage control surgery. J Am Acad Orthop Surg 17: 541-549. Link: https://goo.gl/ub3x7U
- Liu H, Chen W (2011) Images in clinical medicine: fat embolism syndrome. N Engl J Med 364: 1761. Link: https://goo.gl/FDRAq5
- Kim HJ, Lee CH, Lee SH, Cho BM, Kim HK, et al. (2001) Early development of vasogenic edema in experimental cerebral fat embolism in cats: correlation with MRI and electron microscopic findings. Invest Radiol 36: 460-469. Link: https://goo.gl/DWlYxm
Article Alerts
Subscribe to our articles alerts and stay tuned.
 This work is licensed under a Creative Commons Attribution 4.0 International License.
This work is licensed under a Creative Commons Attribution 4.0 International License.
 Save to Mendeley
Save to Mendeley
