Open Journal of Pain Medicine
The analgesic effect of tramadol versus morphine in the treatment of cancer pain in National Cancer Institute, University of Gezira, Sudan (2018)
Ghazi Gasmalla Mohamed Ibrahim1*, Khalid Abbas Owish2 and Mohammed Suliman Zaroug1
2University of Gezira, Public University in Wad Madani, Sudan
Cite this as
Mohamed Ibrahim GG, Owish KA, Zaroug MS (2021) The analgesic effect of tramadol versus morphine in the treatment of cancer pain in National Cancer Institute, University of Gezira, Sudan (2018). Open J Pain Med 5(1): 012-019. DOI: 10.17352/ojpm.000025Cancer pain treatment following the World Health Organization guidelines is effective and feasible. However, the evidence supporting the use of opioids for mild to moderate pain on the Second step of the analgesic ladder is widely discussed. The present assessment compares the efficacy and safety of the use of tramadol in comparison to morphine in the treatment of cancer pain patients. This blind and random study was conducted at the National Cancer Institute at Gezira state in the period from April to October 2018. A total of 100 patients divided into two groups (50 patients for each group) were included in this study. In group one, the patients received tramadol whereas group two received oral morphine and the average dose was 5mg every 4 hours. On the other hand, the average dose of tramadol was 100mg every 6 hours. Our results showed that satisfaction from tramadol was 92%, in other words, 8% were not satisfied, and the most observed side effects were Nausea, Loss of appetite, and Dry mouth. However, morphine satisfaction was 90% while 10% was not satisfied and Nausea, Loss of appetite, and Dry mouth were the most side effects observed. In conclusion, results suggest that tramadol can be used in the treatment of cancer pain, as well as morphine with a slight advantage of tramadol over morphine for the lesser percentage of side effects compared to morphine.
Introduction
Cancer pain can be divided into 3 classes: somatic, visceral, and neuropathic. Somatic and visceral pain results from the activation of nociceptors and are often referred to as “nociceptive pain”. This activation occurs as a result of direct tumor infiltration of the nociception or by the release of inflammatory mediators which stimulate the nociceptors. Somatic pain is usually experienced in the location of the injury whereas visceral pain may be less specific and may be referred to remote sites. On the other hand, neuropathic pain results from injury to the peripheral and/or central nervous system and may persist even after the stimulus has been removed. This type of pain is often perceived as synaesthesia in a region of motor, sensory or autonomic dysfunction and often described as burning, tingling, or electric shock-like [1].
The understanding of these basic concepts is essential for the accurate assessment of pain and in implementing the most appropriate treatment. Most cancer patients will experience pain at some point of the disease and this severity of pain increases proportionally to the severity and cancer stage, and this pain has a major impact on the quality of life of these patients, thus it’s important to study drugs that alleviate this pain. Cancer pain treatment following the World Health Organization guidelines is effective. However, the evidence supporting the use of opioids for mild to moderate pain on the second step of the analgesic ladder is widely discussed. The present evaluation compares the efficacy and safe administration of tramadol and morphine in the treatment of cancer pain [2].
Tramadol is an analgesic medication that has been placed on the 2nd step of the ladder of the WHO Analgesic Ladder for the management of moderately severe cancer pain [3]. (Leppert) Tramadol has a dual mechanism of action. It has μ opioid binding properties (acts as an opioid) and in addition, inhibits the reuptake of serotonin and noradrenaline at the descending inhibitory pathways (hence its efficacy in some neuropathic pain conditions). Tramadol has therefore been found to be a useful drug in patients with cancer pain [4]. Morphine remains a good choice for the management of moderate to severe cancer pain. However, due to strict regulations in many developing countries, it is not readily available. These strict licensing laws and regulations are barriers to the availability of strong opioids in these developing countries. Tramadol is the only readily available opioid analgesic medicine, as it has been placed on a lower schedule compared to potent opioids such as morphine, because of its low abuse potential. [5]. Hence doctors can readily prescribe tramadol to control moderate and severe cancer pain, especially when the pain has mixed characteristics (nociceptive and neuropathic). About 1/3 of patients with cancer pain have pain with neuropathic pain characteristics. And this pain is responding to tramadol [6].
Like most analgesic drugs, there are side effects especially opioid analgesics like morphine and tramadol that may cause extra problems for cancer pain patients.
The variation in responding to analgesic drugs varies according to ethnicity and race and could be affected by the environment.
In a study published in the American Journal of Pain under the title Differences in Pain Coping between Black and White Americans, the study found that there are differences in coping with pain between white and African races[7].
There is a study published on1999 by Stefan Grond, MD, did a comparative study between the high dose of tramadol and the low dose of morphine This study compares and evaluate the efficacy and safety of high doses of oral tramadol (300 mg/d) with low doses of oral morphine (60 mg/d). Patients were included in this no-blinded and nonrandomized study if the combination of a no opioid analgesic and up to 250 mg/d of oral tramadol was inadequate. 810 patients received oral tramadol for a total of 23,497 days, and 848 patients received oral morphine for a total of 24,695 days. The average dose of tramadol was 4286101 mg/d (range 300–600 mg/d); the average dose of morphine was 42613 mg/d (range q10– 60 mg/d).
There are other studies Alternative opioids to morphine in palliative care: a review of current practice and evidence, done by M Barnett-2001- he reviewed the current practice of opioid use in palliative care, conducted from the perspective of a practicing clinician working in the increasingly complex area of symptom control. In examining alternative opioids to morphine. There is a lack of previous studies at the local premises.
Cancer pain
It is estimated that 70% to 90% of patients with advanced cancer experience significant pain. Since uncontrolled pain can have an adverse impact on patients and their families, optimal management of pain should be a priority goal for all clinicians. Cancer pain syndromes can be classified as somatic, visceral, or neuropathic in origin. Pain may be due to tumor infiltration of local structures or to antineoplastic therapy, or it may be unrelated to the tumor [8]. Recognition of pain syndromes is essential for the adequate management of cancer pain. Basic science research on the mechanisms of pain has been helpful in providing the scientific rationale for new approaches to cancer pain management [9].
Pain associated with potentially life-threatening conditions such as cancer is often called malignant pain or cancer pain. However, there is movement toward the use of new terms such as pain associated with human immunodeficiency virus or pain associated with cancer pain includes pain caused by the disease itself like tumor invasion of tissue, compression or infiltration of nerves or blood vessels, organ obstruction, infection, inflammation and/or painful diagnostic procedures or treatments like Biopsy, postoperative pain, toxicities from chemotherapy or radiation treatment [10].
There are several reasons why some experts feel that cancer pain merits a discrete category. First, its acute and chronic components and multiple etiologies make it difficult to classify based on duration or pathology alone. Second, cancer pain differs from chronic no cancer pain in some significant ways like timeframe, levels of pathology, treatment strategies However, there is little evidence to support a distinction between these pain types based on underlying neural processes. Therefore, many pain experts categorize cancer pain as acute or chronic pain [11].
The neurophysiology of cancer pain is complex; it involves inflammatory, neuropathic, ischemic, and compression mechanisms at multiple sites. Knowledge of these mechanisms and the ability to decide if a pain is nociceptive, neuropathic, visceral, or a combination of all three will lead to best practice in pain management.
People with cancer can report the presence of several different anatomical sites of pain which may be caused by the cancer, treatment of cancer, general debility, or concurrent disorders. An accurate and meaningful assessment and reassessment of pain is essential and optimizes pain relief. History, examination, psychosocial assessment, and accurate record keeping should be routine, with pain and quality of life measurement tools used where appropriate [12].
Etiology and types of cancer pain
The experience and expression of pain in the context of active cancer may be affected, among other things, by the psychological state of the individual, their social circumstances, and support. The knowledge that prognosis is limited, or uncertain, gives pain heightened meaning. Cancer patients can experience pain as a direct result of their disease, or indirectly from more general effects of illness, the treatment and unrelated causes. Most disease-related pain is chronic, but patients also experience acute pains and accurate assessment is essential. It is important to recognize that most cancer patients with pain have multiple sites and causes for their pain. Every pain described by the patient must be evaluated and treated individually.
Numerical pain score
Numeric rating scale (NRS) of 1–10 which has been used in this study, is widely used for the assessment of postoperative pain. The numeric rating scale NRS 1–10; 1, no pain; 10, worst pain imaginable has been validated for measuring pain intensity. This scale is often used to divide patients into groups who are in need of pain treatment moderate and severe pain and those who are not mild pain. The presently used treatment threshold or cut-off point for moderate pain treatment is arbitrarily set at NRS≥3,2 3 ≥4,3 4 or ≥5,5–7 and even as high as NRS≥6 in different studies.
objectives
General objectives: To evaluate the clinical effect of tramadol versus morphine and their action in relieving cancer pain in National Cancer Institute (NCI) at Gezira State.
Specific objectives: To estimate the severity of pain and to what degree tramadol compared to morphine lessens the pain in patients with cancer pain in NCI, according to numerical rating scale for pain that used in the research from 1to10.
− To determine the side effects of both tramadol and morphine when used to relive cancer pain in patients suffering from cancer in NCI.
− To compare between tramadol and morphine in terms of efficacy and safety
− To evaluate the satisfaction from tramadol and morphine in relieving cancer pain in patients with cancer in NCI.
Materials and methods
Study design
A comparative observational study was carried out in patients with cancer at NCI, Gezira State, Sudan.
Study area
The study was conducted in the National Cancer Institute of Gezira University at Gezira state, central Sudan. The area of Gezira state is around 8901 square kilometres with a population of 3.5 million distributed in small towns, villages, and camps. Wad Madani is one of the highly populated towns in Sudan and the National Cancer Institute is considered the second largest hospital for cancer treatment in Sudan and the main hospital in Gezira state and other central states. It provides a service of pain treatment for cancer patients as well as a cancer treatment.
Study population
Adult patients with cancer who received either tramadol or morphine for cancer pain relief were the subject of this study.
Sample size
Group 1(n=50) on tramadol
Group2 (n=50) on morphine
A total of (100 patients) were enrolled (50 patients) in the tramadol group and (50 patients) in the morphine group, were selected by stratified random technique to provide information about various comparisons.
Inclusion criteria
Sudanese.
Both sex
Patients aged from 22 – 65years
Taking tramadol or morphine for cancer pain
Exclusion criteria
Non Sudanese patients
Patients who are less 22 – and above 65
Cancer pain patient on drugs rather than tramadol or morphine
Study duration
The study was performed in the period from April 2018- to October 2018.
Data variables
1. Numerical pain score
2. Cancer type
3. Data for Side effects of the tramadol
4. Data for side effects of morphine
5. Data for The dose
6. Data for Frequency of the doses
Data collection
A standard questionnaire was designed for this study. The questionnaire was filled by the patients.
Data analysis
The data were analysed using the Statistical Package for Social Sciences (SPSS) program. The chi-square and t-test were used to compare between different variables and the level of the probability is considered as significant when the p-value is ≤0.05.
Ethical consideration
All participant relatives were assured that all personal information concerning patients’ health status will be kept confidential. The participants were informed about the objective and need of this study.
Permission from the National Cancer Institute administration was granted.
Results
The data were collected through a questionnaire at the National cancer institute of the Gezira University at Gezira state. Descriptive statistics, cross-tabulations (chi-square tests), and t-test have been used to compare the tramadol and morphine in the treatment of cancer pain as shown in the following Table 1:
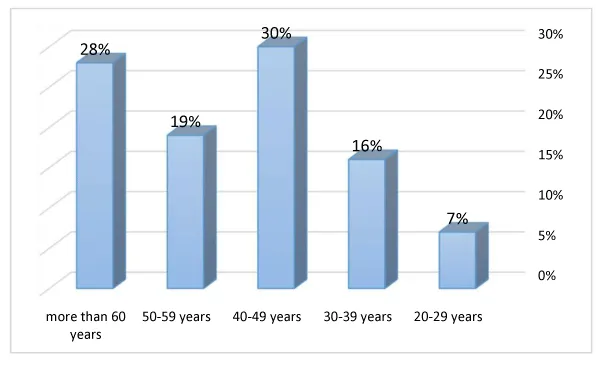
The table above presents the distribution of age groups, (40-49 years) is 30% that means the most patients in the set age (40-49 years) Table 2 Figure 1.
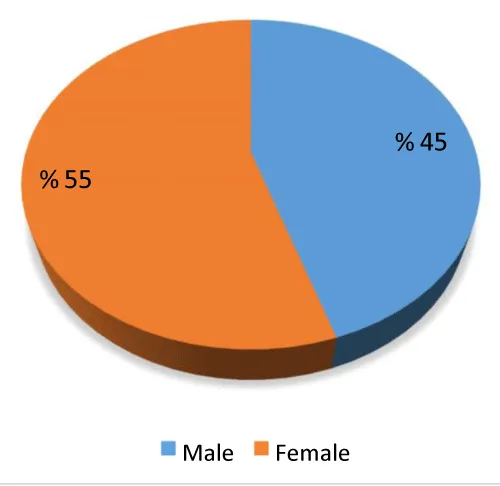
As can be shown in the above table, the gender distribution of the subjects revealed that females have the highest percentage (55%) compared to males (45%) Table 3.
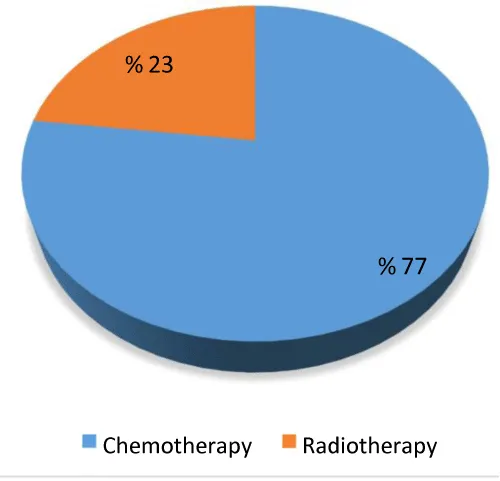
The table above explain that 77% of patients has received Chemotherapy for cancer is used in and 23% has received Radiotherapy Table 4 Figures 2,3.
The table above shows the Correlations between the Numerical pain score before taking the Tramadol & the Numerical pain score after taking the Tramadol, the sig =.001 less than .05 means it correlates with pain score before taking the drug and pain score after taking the drug Table 5.
The table above shows the effect of the Numerical pain score before taking the drug & the Numerical pain score after taking the drug in Tramadol, the sig =.000 less than .05 means it affects the pain score before taking the drug and pain score after taking the drug. The best pain score is after because the pain scores in after decrease compared with before pain score Table 6.
The table above shows the Correlations between the Numerical pain score before taking the Morphine & the Numerical pain score after taking the drug for Morphine, the sig =.000less than .05 means it correlates with the pain score before taking the drug and pain score after taking the drug Table 7.
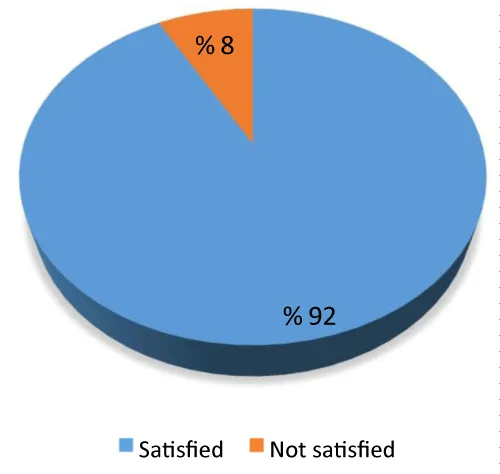
The table above explain the percent of satisfaction from the Tramadol Table 8 Figure 4.
The table above shows the effect of the Numerical pain score before taking the Morphine & the Numerical pain score after taking the Morphine Table 9, the sig =.000 less than .05 means it affects the pain score before taking the Tramadol and pain score after taking the tramadol. The best pain score is after because the pain score after tramadol decreases. Percent of the patients satisfied 92% that means the most patients satisfied with Tramadol Table 9.
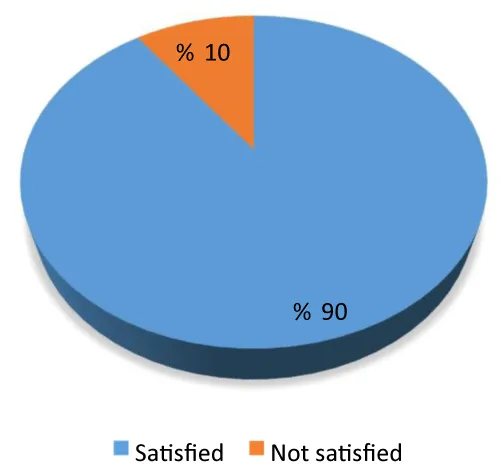
The table above explains the percent of satisfaction from the Morphine, the percent of the patients satisfied 90% that means most of patients satisfied from Morphine Table 10 Figure 5.
The table above explains the distribution of the side effect in Tramadol, Nausea, Loss of appetite, and Dry mouth are the main side effects in tramadol Table 11.
The table above explains the distribution of the side effects in Morphine, Nausea, Loss of appetite, and Dry mouth are the main side effects.
Discussion
Tramadol has been used recently in the control of pain resulting from cancer, patients with cancer pain tend to be in the age of 40years %30 (Table 3) Mary, et al. 2014 reported that there is an increased risk for cancer in middle age males and females, and there is more female patients %55 in this study, the dose of tramadol used for pain control was ranged between 50mg and 150mg and these doses may be considered slightly high in comparison to morphine every six hours which caused satisfaction in most of the patients %92 (Table 8) were satisfied and %8(Table 8) were not satisfied, tramadol showed a significant decrease of pain in patients received it according to numerical pain score after use of tramadol. Tramadol was associated with less frequency of confusion %22 constipation %58 drowsiness %26 and insomnia %50 (Table 10) all these side effects caused by morphine that gives the tramadol the upper hand at this round, tramadol has the advantage of having less frequency of these particular side effects although there is a higher frequency of other side effects nausea %84 loss of appetite %84 dry mouth %84, due to disease in the production rate of saliva, and headache of %62 which considered slightly elevated percentage for a drug supposed to treat pain, but even though tramadol has shown significant control over pain in cancer pain patients
Grond, et al. [5] reported that the use of tramadol in comparison to morphine in the treatment of cancer pain had been significant and it was well tolerated by patients with lesser side effects and safe administration. Morphine still the classic opioid and the first line to be used for cancer pain, the satisfaction from the drug was %90 means it has great control over pain, and not satisfied was %10 at an average dose of 5mg which means a low dose of morphine compared to tramadol dosage used, the side effects were more frequent nausea %90 Smith, et al. 2012 [13] reported that morphine could cause nausea and vomiting with high percentage among all opioid drugs, cough %90, Opioids may also elicit cough by stimulating irritant receptors in tracheal smooth muscle [14]. Constipation %76, and this is due to the opioid receptors in the gastrointestinal tract which tend to decrease bowel motility and peristalsis, laxatives were used in the treatment of this particular side effect but there are excluded from the study results. Loss of appetite %88, although there is no direct evidence of opioid’s effect over the loss of appetite, however loss of appetite has been a common adverse event in cancer pain patients.
Drowsiness %54 central anticholinergic effects of opioids may produce sedation and drowsiness [15-30]. Headache%59.6 may result from hypersensitivity to pain and clinically manifest as tolerance to the opioid drug. Dry mouth %96 and insomnia%58, some evidence regarding affected brain regions and neurotransmitters by which morphine may exert its effects on sleep-wake behavior has emerged. In cats, microinjection of morphine into the medial pontine reticular formation (mPRF) has been found to significantly inhibit REM sleep in a dose- and site-dependent manner (Keifer, et al. 1992). In %58 Kay, et al. 1981 reported that morphine had a high incidence in causing lack or inability to sleep of the patients in the morphine group, morphine had a very high frequency in causing side effects that may interfere with patient quality of life.
Wiffen, et al. [16-47] reported that morphine is an effective analgesic for cancer pain in any patient with any cancer pain.
Conclusion
In conclusion, oral tramadol may have a slight advantage over morphine because it causes fewer or less frequent side effects than morphine, but still has its side effects and still considered an opioid and the headache caused by it is one of the most annoying side effects that may interfere with patient quality of life but could be used for the treatment of cancer pain patients and could be administered safely and could cause excellent pain relief and satisfaction for patients, as for morphine oral tablets is used at small doses and can cause very satisfactory and good control over pain in cancer pain patients but it’s very potent opiate comes at the cost of the long list of side effects some of these side effects may cause real problems.
Recommendations
1. We recommend that Tramadol should be used at the same level as morphine in the treatment of cancer pain patients.
2. The side effects of tramadol or morphine increased proportionally with the dose so whenever it’s necessary to increase the dosage of the drugs we recommend watching out for the severity of side effects.
3. We recommend that the tramadol dose should be calculated very well when used as the first line for cancer pain.
4. Morphine can be a better choice for patients suffering from severe pain or at the late stages of cancer.
5. Tramadol can be a better choice for patients with mild and moderate pain.
6. We recommend treating every patient individually and having a numerical pain score to assess the degree of pain in each patient 7-Pain is not a pleasant sensation so every cancer patient should have some type of pain medication
7. We recommend continuous assessment of pain degree for cancer pain patients to achieve the optimum degree of pain relief.
- Urban D (2009) Critical reviews in oncology hematology. 1st ed. Ireland: 177: 180-181.
- Kopf A (2010) Guide to pain management in low-resource settings. 1st ed. SEATTLE: IASP 137-170. Link: https://bit.ly/3vVCB6y
- WHO's (2013) Cancer Pain Ladder for Adults.” World Health Organization, World Health Organization.
- Scarth E, Smith S (2016) Drugs in Anaesthesia and Intensive Care. 214-231. Link: https://bit.ly/3g8XDId
- Grond S, Radbruch L, Meuser T, Loick G, Sabatowski R, et al. (1999) High-dose Tramadol in comparison to low-dose morphine for cancer pain relief. J Pain Symptom Manage 18: 174-179. Link: https://bit.ly/3ikRc7Q
- Marino PL (2014) Marino's The ICU book. 4th ed. USA: Wolters Kluwer Health/Lippincott Williams & Wilkins 901-908. Link: https://bit.ly/2RsygsK
- Meints SM, Miller MM, Hirsh AT (2016) Differences in pain coping between black and white Americans: A meta-analysis. J Pain 17: 642-653. Link: https://bit.ly/2TEkdRr
- Foley KM (1987) Pain syndromes in patients with cancer. Med Clin North Am 45-54. Link: https://bit.ly/3vTG8Ch
- Regan JM, Peng P (2000) Neurophysiology of cancer pain. Cancer Control 7: 111-119. Link: https://bit.ly/2SXBzIH
- Reis-Pina P, Lawlor PG, Barbosa A (2015) Cancer-related pain management and the optimal use of opioids. Acta Med Port 28: 376-381. Link: https://bit.ly/3fSmC3F
- National Pharmaceutical Council (2001) Pain: current understanding of assessment, management, and treatments. Reston, VA: N.P.C. Inc. Link: https://bit.ly/2T2Y9j1
- Raphael J, Ahmedzai S, Hester J, Urch C, Barrie J, et al. (2010) Cancer pain: part 1: Pathophysiology; oncological, pharmacological, and psychological treatments: a perspective from the British Pain Society endorsed by the UK Association of Palliative Medicine and the Royal College of General Practitioners, Pain Med 11: 742–764. Link: https://bit.ly/3vSC2KM
- Smith HS, Smith JM, Seidner P (2012) "Opioid-induced nausea and vomiting." Ann Palliat Med 1: 121-129. Link: https://bit.ly/2SayJ32
- Bailey PL (1999) Possible Mechanism(s) of opioid-induced coughing. Anaesthesiology 90: 335-335. Link: https://bit.ly/3prO0sn
- Vella-Brincat J, MacLeod AD (2007) Adverse effects of opioids on the central nervous systems of palliative care patients. J Pain Palliat Care Pharmacother 21: 15-25. Link: https://bit.ly/3vVzZWj
- Wiffen PJ, Wee B, Moore RA (2016) Oral morphine for cancer pain. Cochrane Database Syst Rev 4: CD003868. Link: https://bit.ly/3pneefz
- Alsirafy SA, Ibrahim NY, Abou-Elela EN (2012) Opioid Consumption before and after the establishment of A Palliative Medicine Unit in An Egyptian Cancer Centre. J Palliat Care 28: 135–140. Link: https://bit.ly/3chmMzk
- Anon (2018) [EBook]Available at: yan_tramadol_2of2.pdf.
- Barnett M (2001) Alternative opioids to morphine in palliative care: A review of current practice and evidence. Postgrad Med J 77: 371-378. Link: https://bit.ly/3clS0FH
- Barrett KE, Barman SM, Boitan S, Brooks HL, Yuan JX (2012) Ganong’s review of medical physiology (24th ed.). New York, NY: McGraw-Hill Medical. Link: https://bit.ly/3532Yfj
- Benyamin R, Trescot AM, Datta S, Buenaventura R, Adlaka R, et al. (2008) Opioid complications and side effects. Pain Physician 11: S105-S120. Link: https://bit.ly/3iwnxJ1
- Baldini A, Von Korff M, Lin EH (2012) A review of potential adverse effects of long-term opioid therapy. Prim Care Companion CNS Disord 14: PCC.11m01326. Link:
- Bril S, Shoham Y, Marcus J (2011) The ‘Mystery’ of opioid-induced diarrhea. Pain Res Manag 16: 197-199. Link: https://bit.ly/34PyLQM
- Cherny NI (2001) The pharmacological management of cancer pain. European Journal of Cancer 37: 265-278. Link: https://bit.ly/3idUNo6
- Chau D, Walker V, Pai L, Cho LM (2008) Opiates and elderly: Use and side effects. Clin Interv Aging 3: 273-278. Link: https://bit.ly/3yXIYbD
- Elsamra SE, Ellsworth P (2012) Effects of analgesic and anesthetic medications on lower urinary tract function. Urol Nurs 32: 60-67. Link: https://bit.ly/3cjD9LE
- Furlan AD, Sandoval A, Mailis-Gagnon A, Tunks E (2006) Opioids for chronic noncancer pain: A meta-analysis of effectiveness and side effects. CMAJ 174: 1589-1594. Link: https://bit.ly/3poPsMf .
- Gerbershagen H, Rothaug J, Kalkman CJ, Meissner W (2011) Determination of moderate-to-severe postoperative pain on the numeric rating scale: A cut-off point analysis applying four different methods. Br J Anaesth 107: 619-626. Link: https://bit.ly/3fQwpHq
- Gafer N, Elhaj A (2014) Palliative care for cancer patients in Sudan: An overview. Ecancermedicalscience 8: 491. Link: https://bit.ly/3posmWb
- Anita H, Isobel SJ (2011) Core Topics in Pain. Cambridge University Press. Link: https://bit.ly/3uQ8A6R
- "IASP Terminology – IASP (2017) International Association for the Study of Pain (IASP). Last modified December.
- Kay D, Pickworth WB, Neider GL (1981) Morphine-like insomnia from heroin in nondependent human addicts. Br J Clin Pharmacol 11: 159-169. Link: https://bit.ly/3fPbRiG
- Portenoy KR (2018) Up-to-date. [Online] Uptodate.com. Optimizing-analgesia.
- Kumar KH, Elavarasi P (2016) Definition of pain and classification of pain disorders. Journal of Advanced Clinical & Research Insights 3: 87-90. Link: https://bit.ly/3ifDkf3
- Katcher J, Walsh D (1999) Opioid-induced itching. Journal of Pain and Symptom Management 17: 70-72. Link: https://bit.ly/3ijFIl2
- Leppert d. (n.d.). Inclusion of tramadol for cancer pain to the WHO Model List of Essential Medicines (EML).
- Nersesyan H, Slavin KV (2007) The current approach to cancer pain management: Availability and implications of different treatment options. Ther Clin Risk Manag 3: 381–400. Link: https://bit.ly/3ggJrNE
- Osipova NA, Novikov GA, Beresnev VA, Loseva NA (1991) Analgesic effect of tramadol in cancer patients with chronic pain: A comparison with prolonged-action morphine sulphate. C Therapy Res 50: 812-821. Link: https://bit.ly/34Mhec9
- Schug SA, Palmer GM, Scott DA, Halliwell R, Trinca J (2015) Acute pain management: Scientific evidence. Fourth edition 205, Med J Aust 204: 315-317. Link: https://bit.ly/3fTUX2i
- Pickworth WB, Neidert GL, Kay DC (1981) Morphinelike arousal by methadone during sleep. Clinical Pharmacology and Therapeutics 30: 796-804. Link: https://bit.ly/3ijkTGf
- Rausch T, Jansen T (2012) Gastrointestinal Side Effects of Opioid Analgesics. U.S Pharmacist 37: 36–39. Link: https://bit.ly/3wQ2mp4
- Swegle J, Logemann C (2006) Management of Common Opioid-Induced Adverse Effects. Am Fam Physician 74: 1347–1354. Link: https://bit.ly/3z3mF46
- Vissers KC, Besse K, Wagemans M, Zuurmond W, Giezeman MJ, et al. (2011) 23. Pain in patients with cancer. Pain Practice 11: 453-475. Link: https://bit.ly/3pnfD5M
- Westergaard ML, Munksgaard SB, Bendtsen L, Jensen RH (2016) Medication-over use headache A perspective review. Ther Adv Drug Saf 7: 147-158. Link: https://bit.ly/3fSBDCv
- Wilder-Smith C, Schimke J, Osterwalder B, Senn H (1994) Oral tramadol, a μ-opioid agonist and monoamine reuptake-blocker, and morphine for strong cancer-related pain. Ann Oncol 5: 141-146. Link: https://bit.ly/3plIyr7
- Wiffen PJ, Derry S, Moore RA (2014) Impact of morphine, fentanyl, oxycodone or codeine on patient consciousness, appetite and thirst when used to treat cancer pain. Cochrane Database Syst Rev 2014: CD011056. Link: https://bit.ly/2SXCn0b
- White ID, Hoskin PJ, Hanks GW, Bliss JM (1989) Morphine and dryness of the mouth. BMJ 298: 1222-1223. Link: https://bit.ly/3vZUpha
Article Alerts
Subscribe to our articles alerts and stay tuned.
 This work is licensed under a Creative Commons Attribution 4.0 International License.
This work is licensed under a Creative Commons Attribution 4.0 International License.

 Save to Mendeley
Save to Mendeley
