Journal of Surgery and Surgical Research
A rare occurrence: A case report of acute appendicitis and omental infarction unveiled by epigastric pain in a heavy smoker
Med Dheker Touati1,2*, Mohamed Raouf Ben Othmane1,2, Fahd Khefacha1,2, Nadhem Khelifi1,2, Anis Belhadj1,2, Ahmed Saidani1,2 and Faouzi Chebbi1,2
2Faculty of Medicine of Tunis, University of Tunis El Manar, R534+F9H, Street of the Faculty of Medicine, Tunis, Tunisia
Cite this as
Touati MD, Ben Othmane MR, Khefacha F, Khelifi N, Belhadj A, et al. (2023) A rare occurrence: A case report of acute appendicitis and omental infarction unveiled by epigastric pain in a heavy smoker. J Surg Surgical Res 9(2): 009-012. DOI: 10.17352/2455-2968.000156Copyright
© 2023 Touati MD, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.Omental Infarction (OI) is a rare condition that can mimic common causes of acute abdominal pain, primarily affecting individuals aged 40 to 50, with a male predominance. Imaging techniques like ultrasound and computed tomography aid in diagnosis. Treatment options range from conservative management to surgery, depending on severity and complications. OI often leads to right-sided abdominal pain in 90% of cases, with histological features including focal necrosis and fibroblastic reactions.
Acute appendicitis is a common cause of acute abdominal conditions, especially in children and adolescents. Having a patient simultaneously presenting with acute appendicitis and omental infarction is extremely rare, with only three cases reported in the literature to date to our knowledge.
We present the case of a 32-year-old male, a heavy smoker, who presented with epigastric pain and vomiting. Initial clinical suspicion was a perforated ulcer, but imaging revealed swollen appendicitis with adjacent fat stranding and evidence of epiploic infarction near the stomach.
Laparoscopic surgery confirmed the diagnosis of acute appendicitis, with an appendectomy performed and identification of the infarcted omentum, which was preserved. After the operation, the patient had a successful recovery and was discharged on the second postoperative day.
This case firstly emphasizes the rarity of the association between acute appendicitis and omental infarction in the same patient and underscores the importance of considering Omental Infarction (OI) in the differential diagnosis of acute abdominal pain. Imaging plays a crucial role in accurate diagnosis, and a high degree of suspicion and prompt diagnosis are crucial for optimal patient outcomes.
Introduction
Omental Infarction (OI) is a rare condition that can mimic common causes of acute abdominal pain, such as acute appendicitis, cholecystitis, diverticulitis, perforated duodenal ulcer, mesenteric thrombosis, and twisted ovarian cyst [1].
OI tends to occur more frequently in children and in individuals aged 40 to 50 years, with a higher incidence in males compared to females at a 2:1 ratio [2].
Acute appendicitis is a common cause of acute abdomen, especially in children and adolescents who have the highest incidence [3]. Having both acute appendicitis and omental infarction is extremely rare.
The purpose of this case report is to shed light on a rare case of omental infarction associated with acute appendicitis discovered after a presentation characterized by epigastric pain in a smoker patient. This case report highlights the importance of radiological investigations and the success of our conservative treatment approach in dealing with this omental infarction.
Case presentation
We present the case of a 32-year-old male patient with no prior medical or surgical history, who is a heavy smoker, and who presented to the emergency department with progressively worsening epigastric pain for one day, associated with vomiting. There were no associated urinary symptoms. On examination, the patient was hemodynamically stable but had a fever of 38.3 °C. Abdominal examination revealed epigastric tenderness associated with right lower quadrant tenderness, with a negative Rovsing sign. Laboratory tests showed an inflammatory syndrome with a white blood cell count of 18,000/mm3 and a CRP level of 32 mg/L, while lipase levels were normal.
Given the patient's smoking history and epigastric tenderness, the initial suspected diagnosis was a perforated ulcer. To evaluate this further, a chest X-ray focused on the diaphragmatic areas was performed, which did not reveal pneumoperitoneum. A CT scan was then indicated to establish the etiological diagnosis, including the possibility of a perforated ulcer or acute appendicitis.
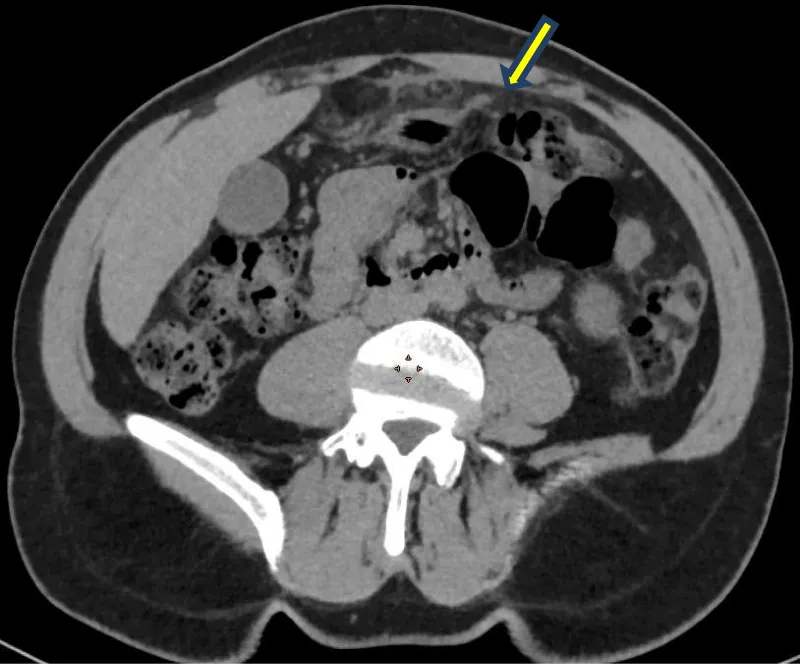
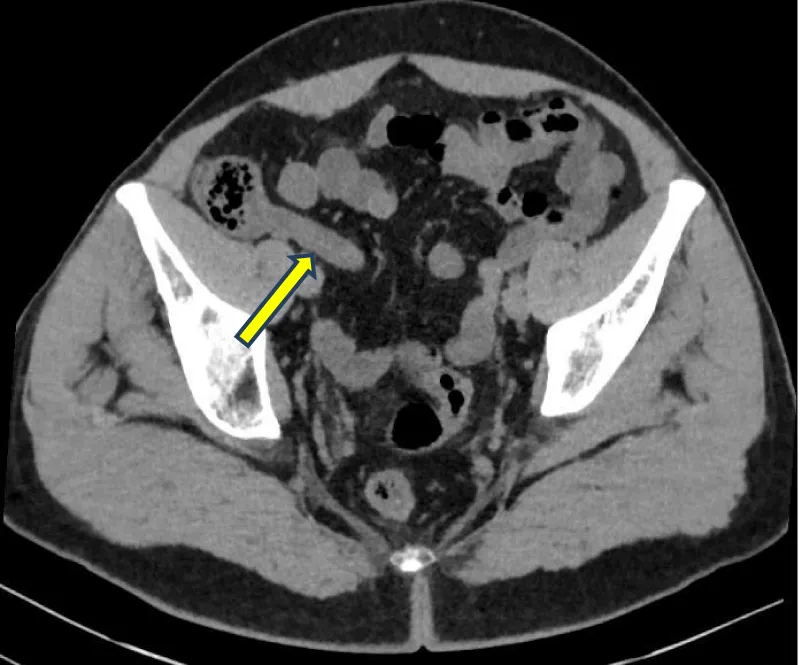
The CT scan showed a swollen, 12mm-wide, internal laterocaecal appendix with adjacent fat stranding. Additionally, there was evidence of epiploic infarction near the stomach (Figures 1,2). After a brief period of resuscitation with intravenous fluids, analgesics, and antibiotics, it was decided to perform laparoscopic surgery.
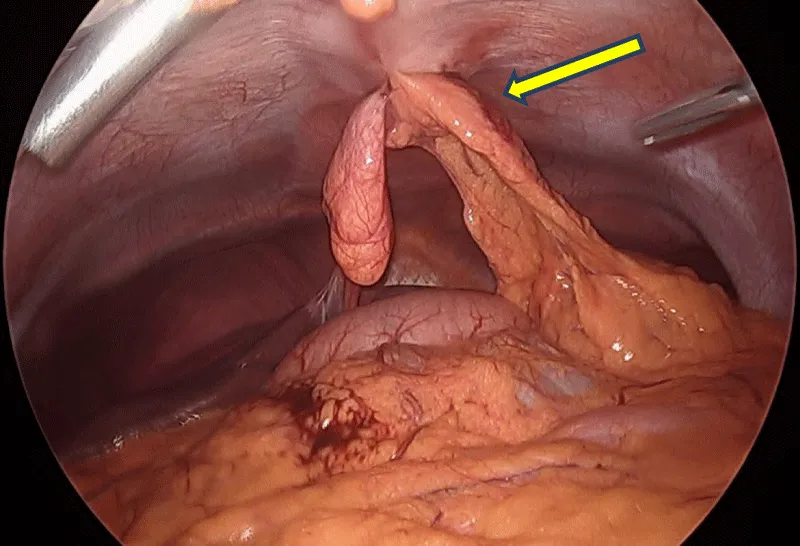
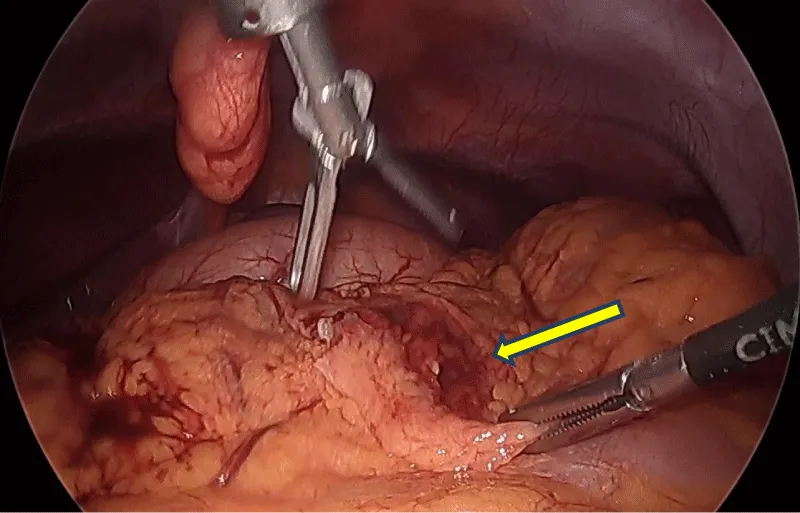
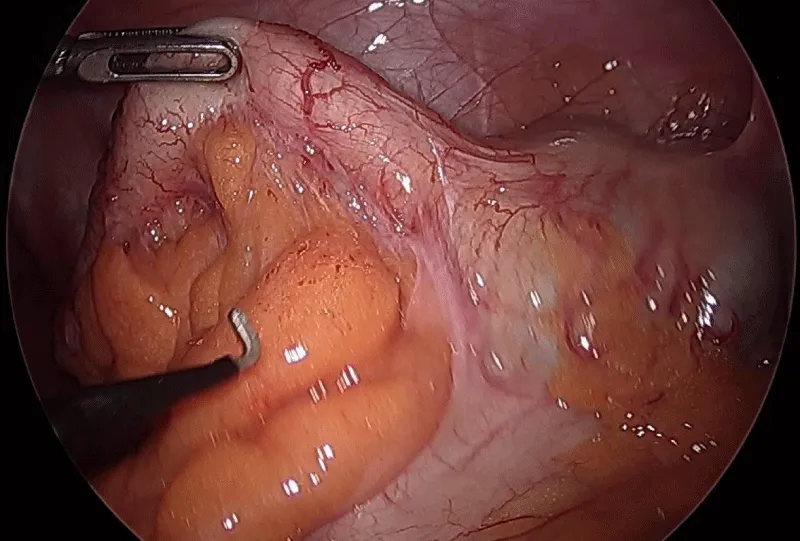
During the exploration, a 4 cm-long epiploic infarction was found in the epigastric region (Figures 3,4), since this omental segment showed no signs of infection or necrosis, it was decided to preserve it without performing an omentectomy and to follow a conservative approach. The exploration was completed by confirming acute appendicitis (Figure 5), and a laparoscopic appendectomy was performed without complications.
In the postoperative period, the patient was kept on analgesics and anti-inflammatories and showed good progress. He was discharged on the second postoperative day. One month after surgery, the patient had a favorable outcome with complete resolution of symptoms.
Discussion
Omental Infarction (OI) is a rare condition that can mimic common causes of acute abdominal pain. It primarily affects individuals aged 40 to 50, with a male predominance [2].
OI predominantly affects the right side of the omentum, resulting in right-sided abdominal pain in 90% of cases [1]. Histological features include focal necrosis and fibroblastic reactions.
Obesity is a well-established risk factor for omental infarction, attributed to the accumulation of fat in the omentum leading to obstruction of blood supply to its distal parts, thereby increasing the risk of torsion [4]. Other risk factors associated with omental infarction, such as polycythemia, hypercoagulability, vasculitis, and conditions predisposing to torsion like trauma, sudden body movements, coughing, heavy food intake, and hyperperistalsis, further contribute to the complexity of this condition [4].
Although rare, an increasing number of cases of omental infarction are reported in recent literature due to the availability of imaging studies, especially computed tomography, even in emergency situations [2,4]. As in our case report, the diagnosis of omental infarction was made preoperatively based on the abdominal CT scan results.
The radiological diagnosis is primarily made through abdominal ultrasound and Computed Tomography (CT scan). Ultrasound features indicative of omental infarction include a non-compressible hyperechoic oval mass, while CT scan results reveal the classic "whirl sign" (whirling patterns of fat and vessels in the omentum) and concentric linear strands or hardening of omental fat [4,5].
Management options vary from conservative treatment to omentectomy in cases of failed conservative management [6].
Currently, there is no consensus on the optimal treatment modality. However, with the increasing prevalence of preoperative diagnosis, conservative treatment is gaining popularity [4]. This approach involves the use of analgesics, anti-inflammatories, and sometimes antibiotics. Surgery may, however, become necessary in case of failure of the conservative approach, particularly in the presence of rare complications such as prolonged pain, abscess formation, and intestinal obstruction [7,8].
In the three cases reported in the literature [9-11] where acute appendicitis was associated with omental infarction, all patients underwent an appendectomy combined with resection of the infarcted omentum. In our particular case, unlike these three cases, the preoperative decision to preserve the infarcted omentum was made to avoid adding morbidity to a condition for which conservative treatment is generally effective. The patient had a straightforward postoperative recovery and was discharged within a day.
The contribution of imaging, especially CT scans, in the preoperative diagnosis of omental infarction lies in its diagnostic precision. Indeed, a typical clinical presentation of appendicitis in a male patient might lead to an immediate McBurney's procedure without resorting to radiological exploration, and the patient could continue to experience unexplained postoperative pain simply because the diagnosis of omental infarction was not established. Not to forget the role of laparoscopy, which also plays a crucial role in these situations, offering the advantage of exploring the entire abdominal cavity.
The pathophysiology of the unique association between omental infarction and acute appendicitis in our patient remains unknown.
Conclusion
The presented case contributes to the limited literature on the coexistence of acute appendicitis and omental infarction, highlighting the importance of thorough diagnostic evaluation and tailored management in these unique clinical scenarios. Imaging, especially in cases with atypical presentations, plays a crucial role. Swift and accurate diagnosis remains essential for optimal patient outcomes, underscoring the need for a high degree of suspicion and prompt intervention.
Patient consent
Written informed consent was obtained from the patient for the publication of this case report and its accompanying images. A copy of the written consent is available for the Editor-in-Chief of this journal to review upon request.
Data availability
The data supporting this case report are available upon request from the corresponding author.
- Suresh CC, Manappallil RG, Chand A, Jayaraj J. Omental infarction: An uncommon aetiology for acute abdomen. Asian Journal of Medical Sciences. 2017;8(1):104‑5.
- Buell KG, Burke-Smith A, Patel V, Watfah J. Omental Infarction: The Great Impersonator. Cureus. 2017 Dec 13;9(12):e1940. doi: 10.7759/cureus.1940. PMID: 29468096; PMCID: PMC5811161.
- Gorter RR, Eker HH, Gorter-Stam MA, Abis GS, Acharya A, Ankersmit M, Antoniou SA, Arolfo S, Babic B, Boni L, Bruntink M, van Dam DA, Defoort B, Deijen CL, DeLacy FB, Go PM, Harmsen AM, van den Helder RS, Iordache F, Ket JC, Muysoms FE, Ozmen MM, Papoulas M, Rhodes M, Straatman J, Tenhagen M, Turrado V, Vereczkei A, Vilallonga R, Deelder JD, Bonjer J. Diagnosis and management of acute appendicitis. EAES consensus development conference 2015. Surg Endosc. 2016 Nov;30(11):4668-4690. doi: 10.1007/s00464-016-5245-7. Epub 2016 Sep 22. PMID: 27660247; PMCID: PMC5082605.
- Barai KP, Knight BC. Diagnosis and management of idiopathic omental infarction: A case report. Int J Surg Case Rep. 2011;2(6):138-40. doi: 10.1016/j.ijscr.2011.02.014. Epub 2011 Apr 5. PMID: 22096707; PMCID: PMC3199678.
- Itenberg E, Mariadason J, Khersonsky J, Wallack M. Modern management of omental torsion and omental infarction: a surgeon's perspective. J Surg Educ. 2010 Jan-Feb;67(1):44-7. doi: 10.1016/j.jsurg.2010.01.003. PMID: 20421090.
- Lindley SI, Peyser PM. Idiopathic omental infarction: One for conservative or surgical management? J Surg Case Rep. 2018 Mar 26;2018(3):rjx095. doi: 10.1093/jscr/rjx095. PMID: 29599961; PMCID: PMC5868192.
- Rimon A, Daneman A, Gerstle JT, Ratnapalan S. Omental infarction in children. J Pediatr. 2009 Sep;155(3):427-431.e1. doi: 10.1016/j.jpeds.2009.03.039. Epub 2009 Jun 21. PMID: 19540514.
- Park TU, Oh JH, Chang IT, Lee SJ, Kim SE, Kim CW, Choe JW, Lee KJ. Omental infarction: case series and review of the literature. J Emerg Med. 2012 Feb;42(2):149-54. doi: 10.1016/j.jemermed.2008.07.023. Epub 2008 Dec 20. PMID: 19097725.
- Koay HT, Mahmoud HE. Simultaneous omental infarction and acute appendicitis in a child. Med J Malaysia. 2015 Feb;70(1):42-4. PMID: 26032530.
- Mani VR, Razdan S, Orach T, Kalabin A, Patel R, Elsaadi A, Sullivan K, Gattorno F. Omental Infarction with Acute Appendicitis in an Overweight Young Female: A Rare Presentation. Case Rep Surg. 2019 Apr 7;2019:8053931. doi: 10.1155/2019/8053931. PMID: 31093415; PMCID: PMC6476035.
- Battaglia L, Belli F, Vannelli A, Bonfanti G, Gallino G, Poiasina E, Rampa M, Vitellaro M, Leo E. Simultaneous idiopathic segmental infarction of the great omentum and acute appendicitis: a rare association. World J Emerg Surg. 2008 Oct 29;3:30. doi: 10.1186/1749-7922-3-30. PMID: 18959804; PMCID: PMC2605737.
Article Alerts
Subscribe to our articles alerts and stay tuned.
 This work is licensed under a Creative Commons Attribution 4.0 International License.
This work is licensed under a Creative Commons Attribution 4.0 International License.


 Save to Mendeley
Save to Mendeley
