Journal of Surgery and Surgical Research
A case report of tubular apocrine adenoma of lower eyelid
Michele Altieri1*, F Giacomelli1 and L Anselmi2
2Pathology Unit, Villa Scassi Hospital, ASL 3, Genova, Italy
Cite this as
Altieri M, Giacomelli F, Anselmi L (2023) A case report of tubular apocrine adenoma of lower eyelid. J Surg Surgical Res 9(2): 005-008. DOI: 10.17352/2455-2968.000155Copyright
© 2023 Altieri M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.Moll glands are sweat apocrine glands close to the eyelid margin. Tumors derived from Moll glands are rare, although Moll glands cysts are frequent. They originate from their glandular tissue or tubules. In this report we present a rare case of a lower eyelid skin tubular apocrine adenoma occurred in the right eye lower eyelid of a caucasian 45 year old woman.
The lesion was nodular and dome shaped and its size was 1.5 × 3.5 × 2 mm. After a complete excision the lesion was analyzed by our pathology unit.
Histologic sections were stained with haematoxylin and eosin, alcian blue, periodic acid-Schiff (PAS). Additionally, the following immunohistochemical markers were used: cytokeratin 7 (CK7), cytokeratin 8/18 (CK8/18), cytokeratin 20 (CK20), S-100 protein and gross cystic disease protein 15 (GCDFP-15) (4,5).
The immunohistochemical and phenotypic features resulted suggest the diagnosis of lower eyelid tubular apocrine adenoma probably originated from Moll glands.
These findings allowed us to diagnose a very rare and benign cutaneous lesion of eyelid skin.
Introduction
Sweat glands present in the eyelids are both apocrine and eccrine. The apocrine glands are bigger than the eccrine and are characterized by a deeply eosinophilic columnar to cuboidal epithelium with basal nuclei and apical cytoplasmic snouts of “cellular decapitation” secretion [1-5].
The eccrine glands are described as lined by low, cuboidal, or flattened epithelium [1,2].
The apocrine glands were described and named by the Dutch ophthalmologist Jacob Moll (1832-1914) [1].
They are present close to the eyelid margin [1-5] and from their epithelium can derive benignly (adenomas) and malignant (adenocarcinomas) tumors [3].
It is also reported that true neoplasms originating from sweat glands (both apocrine and eccrine) are rare [1,2] although Moll’s glands cysts are relatively frequent [1-5].
A tubular apocrine adenoma or tubular papillary adenoma characterized by an apocrine differentiation is to be considered a rare benign sweat apocrine gland tumor. These neoplasms are most commonly found as a nodular solitary lesion of the scalp [6].
Despite numerous apocrine glands being present in the eyelids, very few benign tumors with apocrine origin have been reported at these locations, besides hidrocystomas which are found along the eyelid margins and canthi [1].
According to the World Health Organization (WHO) classification of apocrine tumors we can consider synonyms terms such as apocrine adenoma, tubular adenoma, tubulopapillary hidradenoma, and papillary tubular adenoma [7,8].
In this report, we present a rare case of a lower eyelid skin tubular apocrine adenoma that occurred in a caucasian 45-year-old woman.
Case report
A 45-year-old caucasian woman patient was referred to the ophthalmic plastic clinic of our hospital due to a skin growth on her lower right eyelid of six month’s duration.
The lesion was dome shape, sessile, well-circumscribed, skin-colored, and nonulcerated whose size was 1.5 × 3.5 × 2 mm (Figure 1).
The patient underwent a full slit lamp assessment with funduscopy in both eyes and all findings were normal. Her general health (in relation to blood pressure, full blood count, metabolism) was normal too. In the past, she did not undergo any previous surgery on the eyeball and she was not on any medical treatment. The patient was not aware of any known allergies.
An excisional biopsy was then performed. The surgical wound was immediately sutured with a 6/0 silk interrupted suture to be removed 5 days after the biopsy. A Tobramicine 0,3% ointment was prescribed bd. for 3 days. The specimen had a well-demarcated surface and it was not encapsulated. It was sent to our Pathology Unit for histological examination.
The patient underwent an ophthalmic plastic assessment 5 days after the surgery. Then she was assessed one month, 6 months, 12 months, and 24 months after the surgery by our ophthalmic plastic unit.
Histologic sections were stained with hematoxylin and eosin, alcian blue, and periodic acid-Schiff (PAS). Additionally, the following immunohistochemical markers were used: cytokeratin 7 (CK7), cytokeratin 8/18 (CK8/18), cytokeratin 20 (CK20), S-100 protein, and gross cystic disease protein 15 (GCDFP-15) [9-11].
The operated eyelid showed a quick and full recovery process after the excisional surgery.
There was not any recurrence during the 24-month follow-up.
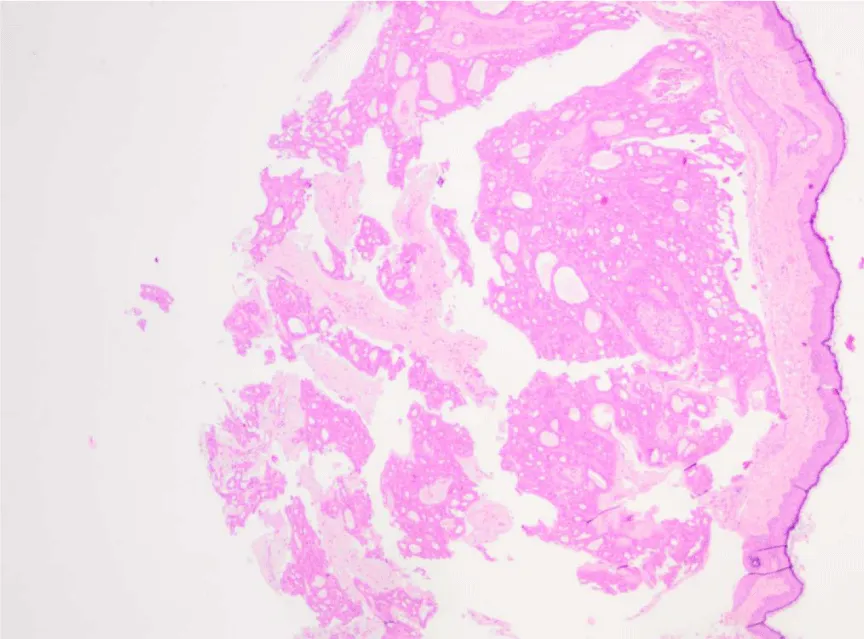
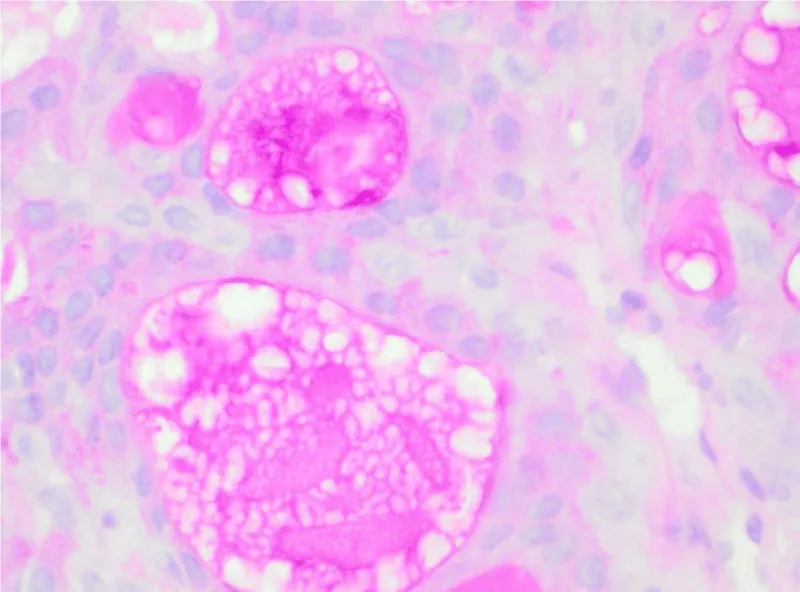
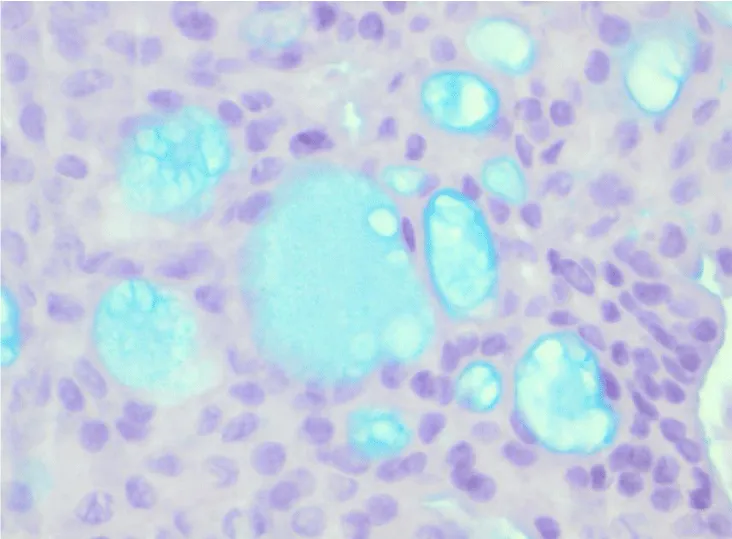
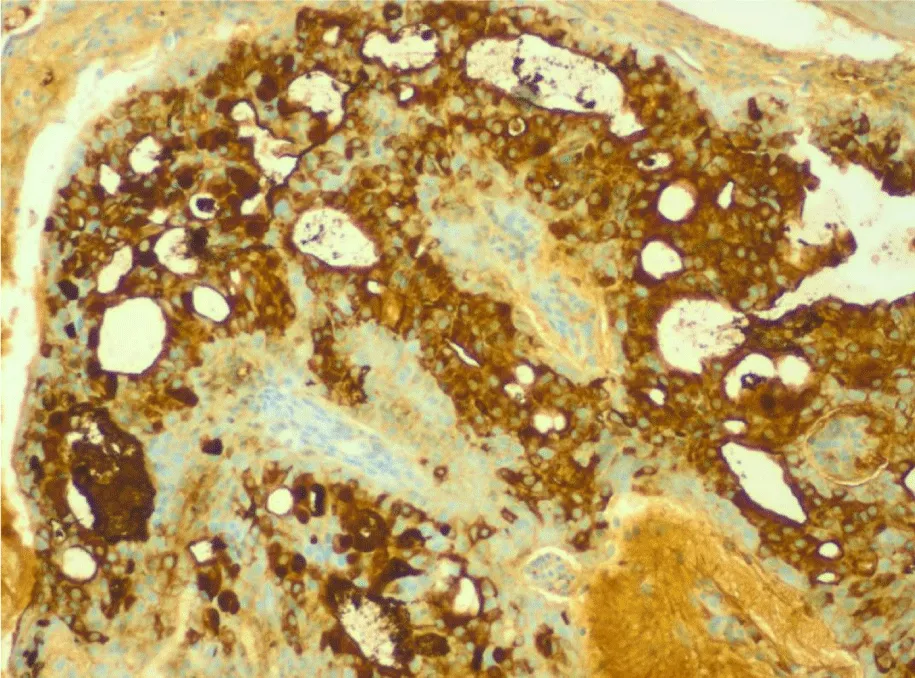
The histological examination done on multiple sections after histochemical and immunohistochemical staining showed a chorion neoformation composed of different sizes with two layers of columnar cell tubules (Figure 2). The neoformation contains areas of myxoid stream change (positive to PAS) (Figure 3) and Alcian Blue (Figure 4) and in the tubular cells ducts mucin was present too.
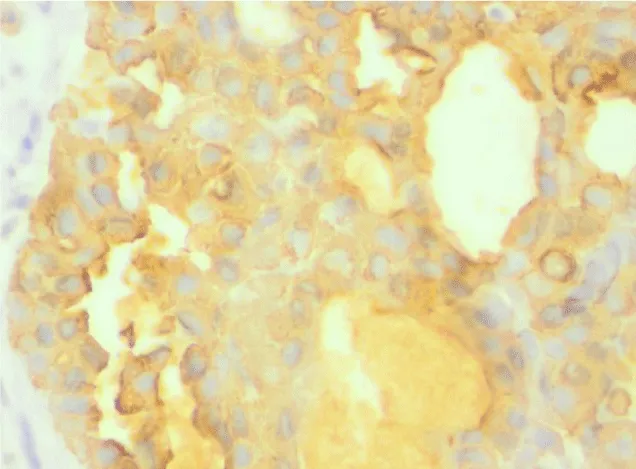
Immunohistochemical analysis showed positivity to CK 7 (Figure 5), CK 8/18 (Figure 6), (focal positivity of membrane and cytoplasm), and GCDFP-15 (Figure 7). However, there was negativity to CK 20 (Figure 8) and to protein S-100 (Figure 9). These immunohistochemical and phenotypic features suggest the diagnosis of flower eyelid tubular apocrine adenoma probably originated from Moll glands [3-5,9].
The authors declare that the study complies with the guidelines for human studies. The subject has given informed consent. The authors declare also that there are no financial interests or conflicts of interest related to this case report.
Discussion
Human apocrine glands are deriving during puberty from eccrine precursors in the axilla, scalp, and pubic areas. They are rare in the ocular adnexa. Although cysts of Moll's glands are common, true neoplasms are rare, and malignant tumors deriving from those glands are very rare [9,10].
Moll’s gland tumors are generally derived from glandular tissue of tubules that usually comprise two layers. The inner cells generally retain the characteristic secretary appearance of apocrine sweat glands, though squamous metaplasia also occurs. The outer layer consisting of small spindle cells is thought to represent the myoepithelium of a normal gland [4].
Apocrine mixed tumors of the skin occur frequently on the face and neck but are rare in the eyelid [4].
Apocrine glandular function is unknown, but research suggests that protein-bound hexanoic acids are released by cutaneous diphtheroids, producing mammalian pheromones [9,10].
The histopathological examination of this lower eyelid lesion, apparently very common and not so clinically important, allowed us to diagnose a very rare cutaneous lesion of eyelid skin.
From the macroscopic clinical point of view, the lesion described in this report, like most tumors of Moll's glands is small and asymptomatic. Clinically they can be often misdiagnosed as cysts, papillomas, fibromas, molluscum contagiosum, seborrheic keratosis, and other benign lesions but also as basal cell carcinoma [4,5,9-11].
In the leading literature, there are only a few reports of skin eyelid tubular apocrine adenoma.
The histologic features of this eyelid lesion are described with lobules of well-differentiated tubular structures present most commonly at the dermis and less frequently at the subcutis [11-14].
The occurrence of tubular apocrine adenoma is more frequent in females in comparison to males with a ratio of 2:1 [15].
The adenocarcinomas deriving from Moll's glands are very rare but also very aggressive neoplasms showing local invasiveness and possible production of lymphatic and haematic metastasis, with a very unfavorable “quoad valetudinem” prognosis (with mandatory aggressive surgery such as orbital exenteration) and sometimes unfavorable “quoad vitam” prognosis (intracranial extensions of the lesion producing the death of the patient are reported) [9,10].
Conclusion
We can state that eye surgeons are often challenged in the diagnosis of this rare neoplasm. The eyelid location is to be considered ectopic.
The histopathological analysis with immunohistochemistry findings is mandatory for the correct diagnosis. These analyses require a qualified Pathology Unit that is supposed to work with direct contact with the Ophthalmology Unit.
A complete excision of the lesion must be done. Some recurrences after incomplete excision are reported.
- Abbeel L, Van Ginderdeuren R. Ectopic Tubular Papillary Apocrine Adenoma on the Eyelid: A Case Report of Misleading Clinical Presentation and Location. Ocul Oncol Pathol. 2018 Sep;4(5):267-271. doi: 10.1159/000485426. Epub 2018 Feb 6. PMID: 30320096; PMCID: PMC6167663.
- Jakobiec FA, Zakka FR. A reappraisal of eyelid eccrine and apocrine hidrocystomas: microanatomic and immunohistochemical studies of 40 lesions. Am J Ophthalmol. 2011 Feb;151(2):358-74.e2. doi: 10.1016/j.ajo.2010.08.028. Epub 2010 Dec 18. PMID: 21168812.
- Gates O, Warren S, Warvi WN. Tumors of Sweat Glands. Am J Pathol. 1943 Jul;19(4):591-631. PMID: 19970710; PMCID: PMC2033085.
- Ni C, Wagoner M, Kieval S, Albert DM. Tumours of the Moll's glands. Br J Ophthalmol. 1984 Jul;68(7):502-6. doi: 10.1136/bjo.68.7.502. PMID: 6329262; PMCID: PMC1040390.
- HEADINGTON JT. Mixed tumors of skin: eccrine and apocrine types. Arch Dermatol. 1961 Dec;84:989-96. doi: 10.1001/archderm.1961.01580180105016. PMID: 13905736.
- Landry M, Winkelmann RK. An unusual tubular apocrine adenoma. Arch Dermatol. 1972 Jun;105(6):869-79. PMID: 4113017.
- LeBoit PE, Burg G, Weedon D, Sarasain A (eds): World Health Organisation Classification of Tumors; Pathology and Genetics of Skin Tumors. Lyon, IARC Press, 2066; 145-146.
- Elder DE, Massi D, Scolyer RA, Willemze R. WHO Classification of Skin Tumours; International Agency for Research on Cancer: Lyon, France, 2018. ISBN 978-92-832-2440-2.
- Barker-Griffith AE, Streeten BW, Charles NC. Moll gland neoplasms of the eyelid: a clinical and pathological spectrum in 5 cases. Arch Ophthalmol. 2006 Nov;124(11):1645-9. doi: 10.1001/archopht.124.11.1645. PMID: 17102015.
- Laver NM, Hidayat AA, Croxatto JO. Pleomorphic adenocarcinomas of the ciliary epithelium. Immunohistochemical and ultrastructural features of 12 cases. Ophthalmology. 1999 Jan;106(1):103-10. doi: 10.1016/S0161-6420(99)90024-6. PMID: 9917789.
- Ito T, Nomura T, Fujita Y, Abe R, Shimizu H. Tubular apocrine adenoma clinically and dermoscopically mimicking basal cell carcinoma. J Am Acad Dermatol. 2014 Aug;71(2):e45-6. doi: 10.1016/j.jaad.2014.01.873. PMID: 25037809.
- Choi J, Seo JH, Choi JY, Seo BF, Kwon H, Jung SN. Apocrine tubular adenoma on the palm: A case report. Medicine (Baltimore). 2021 Dec 10;100(49):e28002. doi: 10.1097/MD.0000000000028002. PMID: 34889245; PMCID: PMC8663837.
- Macagno N, Sohier P, Kervarrec T, Pissaloux D, Jullie ML, Cribier B, Battistella M. Recent Advances on Immunohistochemistry and Molecular Biology for the Diagnosis of Adnexal Sweat Gland Tumors. Cancers (Basel). 2022 Jan 18;14(3):476. doi: 10.3390/cancers14030476. PMID: 35158743; PMCID: PMC8833812.
- Eiger-Moscovich M, Zhang PJL, Lally SE, Shields CL, Eagle RC Jr, Milman T. Tubular apocrine adenoma of the eyelid - A case report and literature review. Saudi J Ophthalmol. 2019 Jul-Sep;33(3):304-307. doi: 10.1016/j.sjopt.2019.07.005. Epub 2019 Jul 26. PMID: 31686976; PMCID: PMC6819710.
- Attafi S, Smichi I, Rkik W. Tubular apocrine adenoma of the axilla: a rare adnexal tumor. Our Dermatol Online 2015; 6:360-1.
Article Alerts
Subscribe to our articles alerts and stay tuned.
 This work is licensed under a Creative Commons Attribution 4.0 International License.
This work is licensed under a Creative Commons Attribution 4.0 International License.



 Save to Mendeley
Save to Mendeley
