Journal of Surgery and Surgical Research
Denture in the rectum: A case report
Aymen Al-Roubaie* and Jacques Perry
Cite this as
Al-Roubaie A, Perry J (2022) Denture in the rectum: A case report. J Surg Surgical Res 8(1): 009-012. DOI: 10.17352/2455-2968.000147Copyright
© 2022 Al-Roubaie A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.Swallowed foreign bodies are uncommon during general anesthesia. In the majority of the cases, these foreign bodies are passed spontaneously and uneventfully and the minority requires endoscopic or surgical intervention. It is recommended that every removable prosthesis should be removed, labeled, and stored in a safe place preoperatively. Furthermore, if a foreign body was missing, proper notification should be done in the immediate postoperative period to enable early detection and avoid any complications that might result from its impaction in distal places. This paper reports a case of a swallowed denture during induction of anesthesia. The clinical and imaging findings are presented along with a review of the literature. A 53-year old woman was admitted for laparoscopic cholecystectomy. A week postoperatively, the patient reported a colicky lower abdominal pain increasing in severity. Lower quadrants deep tenderness was elicited by examination. A foreign body was detected within the proximal rectum by abdominal CT scan. The foreign body was the patient’s denture that was not removed earlier during the induction of anesthesia. Endoscopic foreign body removal was done by flexible sigmoidoscopy. This case report highlights the importance of removing any removable prosthesis before induction of anesthesia and reporting any missing prosthesis such as dentures in the immediate postoperative period.
Introduction
Swallowed Foreign Body (FB) in adults is an important issue in different specialties like general surgery, anesthesia, gastroenterology, and psychiatry and usually happens in an adult with psychiatric problems, poorly fitted dentures, or during general anesthesia [1]. It is usually infrequently encountered in adults and in most cases, the FB represents a swallowed bone of fish or chicken [2]. The diagnosis depends on a proper history and examination and is supported by imaging modalities by anticipated FB character [3-6]. Although in 80% of cases FB passed with a conservative approach, 20% required endoscopic intervention. Less than 1% required surgical intervention [3,4,6-8]. It is recommended to remove any removable prosthesis like denture preoperatively and stored it after labeling in a safe place. In the present case, the denture was swallowed and migrated through the gastrointestinal tract smoothly and impacted in the rectum Figures 1-3. Failure of proper notification of missing denture post-operatively which might result in early detection of FB in the esophagus or stomach with subsequent early removal rendered the patient at more risk when the FB might cause perforation or intestinal obstruction through its journey in the gastrointestinal tract. Foreign body entrapment in the rectum is not uncommon. Depending on the level of entrapment, a FB may cause damage to the rectum, rectosigmoid, or descending colon. Fortunately, in our case, there was no perforation in the rectum and the patient was recovered uneventfully post removal.
The author reports a case of a FB in the rectum two weeks post-operative laparoscopic cholecystectomy. The foreign body was the patient’s denture which was not removed earlier during the induction of anesthesia.
Case presentation
A fifty-three years old lady presented with lower abdominal pain for seven days. The pain was colicky, increasing in severity over the last few days. Neither vomiting nor constipation has been reported. However, the patient described burning pain during defecation. There was no bleeding per rectum before or after motion. Fever was noted intermittently but was responding to paracetamol. The patient had laparoscopic cholecystectomy 2 weeks ago performed under uneventful general anesthesia. The patient reported a missing denture post-operatively. During induction, a decision was made not to remove her denture as it seemed fixed well. She was advised that she had vomited post-operatively and apparently, she had lost the denture in the vomitus. However, there was no confirming evidence of its presence in the vomitus. The patient has no other medical history and is not on any regular medications. On examination, she was in pain with normal vital signs. Abdominal examination revealed a soft abdomen with lower quadrants deep tenderness. There was no guarding or rigidity and after the patient’s consent, a digital rectal exam in the presence of a chaperone was done with no mass or bleeding appreciated. Her blood results showed raised inflammatory markers with a white cell count of 16.31×109 L (normal 4−11×109 L) and a C reactive protein of 112 mg/L (normal <5 mg/L). Her other blood tests including hemoglobin, renal function, liver function, lactate, and lipase were within normal limits.
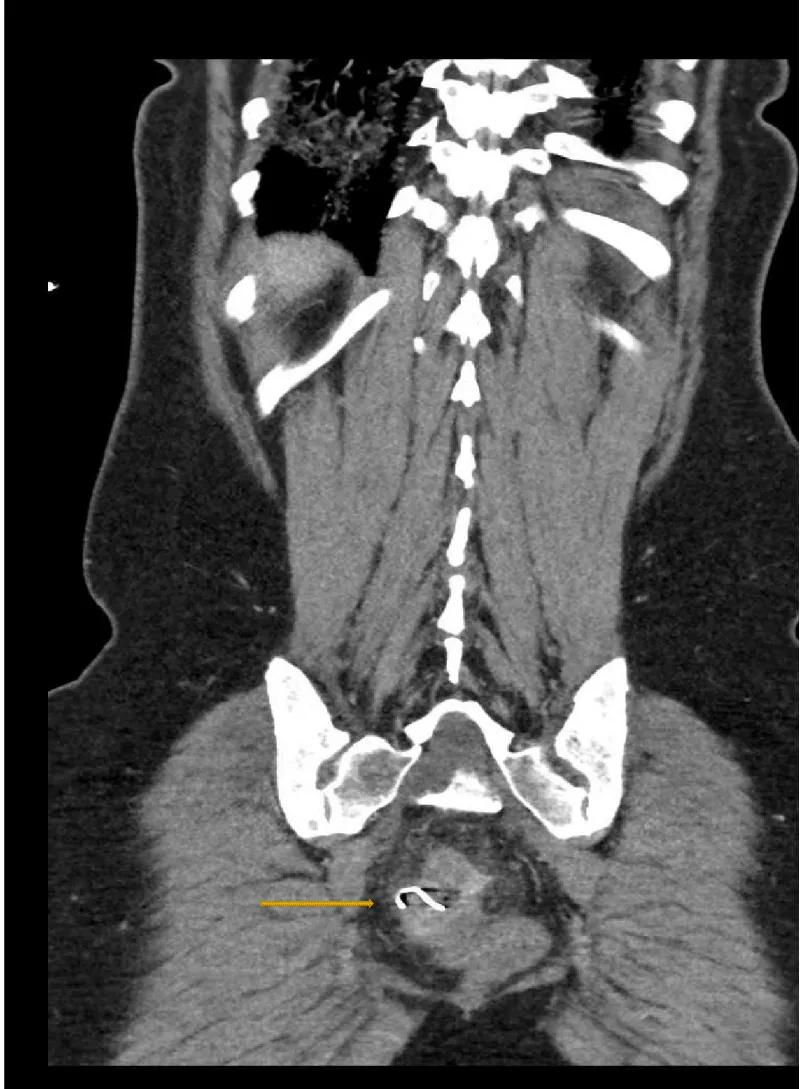
Computerized tomography scan showed two metallic density curved linear structures measuring approximately 2 cm each on either side of the rectal wall with mild perirectal stranding and rectal wall thickening. There is no evidence of free gas or drainable collection Figures 1,2.
The patient was admitted under the general surgery department with a plan for manual or endoscopic FB removal. She was commenced on wide spectrum antibiotics and kept nil by mouth. During the operation, manual removal failed. Therefore, rigid sigmoidoscopy was tried with no good visualization. However, using the flexible sigmoidoscopy enhanced proper visualization of the FB high in the rectum Figure 3. The FB was retrieved endoscopically by snare with no reported rectal damage or perforation Figure 4. Postoperatively the patient was observed in the ward with next blood tests showed trending down of CRP and WBC and been discharged after one day. The patient was followed up in the surgical clinic with normal biochemical markers, examination, and imaging in two weeks.
Discussion
Foreign bodies usually migrated in the gastrointestinal tract safely after ingestion. In 99% of cases, foreign bodies were reported to be seen in the stool with no complications. However, complications have been described in 1% [9,10]. Foreign bodies can be trapped anywhere in the gastrointestinal tract, but they are most commonly documented in the narrowing parts such as the pylorus, ileocecal valve, and sigmoid colon in addition to the area of angulation like the rectosigmoid valve [11,12].
The usual presentations of gastrointestinal foreign bodies are abdominal pain, bleeding, obstruction, collection, or perforation [13]. In our case, the presentation was abdominal pain associated with mild fever but no perforation or collection.
Treatment depends mainly on the type of foreign body, its consistency, location, and whether complication has happened or not. For example, foreign bodies who has spikes or are long and thin tend to cause complications such as fish bones or hooks of dentures [2]. While in the majority of cases, watchful waiting with serial x-rays are the treatment of choice as most of them will be expelled in the stool. Endoscopic intervention is required in 20% and further formal surgical intervention is required in less than 1% [3,4,6,14-19].
In our case, the foreign body has impacted the sigmoid colon with two sharp ends and the patient was symptomatic. Two treatment options were available either endoscopic or formal surgical removal after the failure of manual removal because the FB was high in the sigmoid colon. Minimal invasive techniques together with simplicity and reduction of post-operative recovery time have made endoscopic options more efficient and feasible [6]. However, retrieval of foreign bodies in the rectum using endoscopy is challenging [9,10].
There are few cases of successful endoscopic removal of rectal foreign bodies without surgeries ref [20-27].
Another case report was able to remove rectal foreign body using a custom-made giant snare [23].
The author reported successful removal of the rectal foreign body using the snare with no complications. The denture was around 2 cm in diameter with two sharp ends and that’s probably explained why it was impacted in the rectum and did not pass with a normal motion movement. In our case, the post-operative recovery time was one day, and the patient was followed with further images and blood tests in 14 days which were normal.
Preoperative removal of any prosthesis is crucial, and it was necessary in our case to avoid any risk of complications as well as the cost of rehospitalization. Early notification and seeking of medical attention are cardinal in any missing foreign bodies because dealing with foreign bodies in the upper gastrointestinal tract reduce the risk of foreign bodies' impaction in a more difficult and narrow part of the gastrointestinal tract or the risk of causing perforation during its journey.
Conclusion
It's fundamental to remove any prosthesis preoperatively like a denture and to report any missing prosthesis postoperatively promptly to avoid any future risk of impacted FB or delayed presentation which might put the patient at risk. Endoscopic removal was feasible and prevented the patient from a more invasive procedure like a laparoscopic or open approach.
- De Ruiter MH, Van Damme PA, Drenth JP (2008) Serious complications following (removal after) ingestion of a partial denture. Ned Tijdschr Tandheelkd 115: 267–270.Link: https://bit.ly/3NxENKH
- Nandi P, Ong GB (1978) Foreign body in the oesophagus:review of 2394 cases. Br J Surg 65: 5–9. Link: https://bit.ly/3ISbQpk
- Webb WA (1995) Management of foreign bodies of the upper gastrointestinal tract: update. Gastrointest Endosc 41: 39–51. Link: https://bit.ly/3Lljt9s
- Ginsberg GG (1995) Management of ingested foreign objects and food bolus impactions. Gastrointest Endosc 41: 33–38. Link: https://bit.ly/3LmSnyD
- Chiu YH, Hou SK, Chen SC, How CK, Lam C, et al. (2012) Diagnosis and endoscopic management of upper gastrointestinal foreign bodies. Am J Med Sci 343: 192–195. Link: https://bit.ly/36uTSwc
- Ikenberry SO, Jue TL, Anderson MA, Appalaneni V, Banerjee S, et al. (2011) Management of ingested foreign bodies and food impactions. Gastrointest Endosc 73: 1085–1091. Link: https://bit.ly/3JNxnRu
- Sung SH, Jeon SW, Son HS, Kim SK, Jung MK, et al. (2011) Factors predictive of risk for complications in patients with oesophageal foreign bodies. Dig Liver Dis 43: 632–635. Link: https://bit.ly/3iKtv7K
- Peng A, Li Y, Xiao Z, Wu W (2012) Study of clinical treatment of esophageal foreign body-induced esophageal perforation with lethal complications. Eur Arch Otorhinolaryngol 269: 2027–2036. Link: https://bit.ly/3wLr8tQ
- Rodríguez-Hermosa JI, Codina-Cazador A, Sirvent JM, Martín A, Gironès J, et al. (2008) Surgically treated perforations of the gastrointestinal tract caused by ingested foreign bodies. Colorectal Dis 10: 701–707. Link: https://bit.ly/3tMQHIN
- Velitchkov NG, Grigorov GI, Losanoff JE, Kjossev KT (1996) Ingested foreign bodies of the gastrointestinal tract: retrospective analysis of 542 cases. World J Surg 20: 1001–1005. Link: https://bit.ly/3JQOima
- Madrona AP, Hernandez JAF, Prats MC, Riquelme JR, Paricio PP (2000) Intestinal perforation by foreign bodies. Eur J Surg 166: 307–309. Link: https://bit.ly/3IPbJuO
- Li ZS, Sun ZX, Zou DW, Xu GM, Wu RP, et al. (2006) Endoscopic management of foreign bodies in the upper-GI tract: experience with 1088 cases in China. Gastrointest. Endosc 64: 485–492. Link: https://bit.ly/3LmTiz5
- Bekki T, Fujikuni N, Tanabe K, Amano H, Noriyuki T, et al. (2019) Liver abscess caused by fish bone perforation of stomach wall treated by laparoscopic surgery: a case report. Surg Case Rep Rev 5: 79. Link: https://bit.ly/3NpL4IB
- Cheng W, Tam PK (1999) Foreign-body ingestion in children: experience with 1,265 cases. J Pediatr Surg 34: 1472–1476. Link: https://bit.ly/35ixCF0
- Smith MT, Wong RK (2007) Foreign bodies. Gastrointest Endosc Clin N Am 17: 361–382. Link: https://bit.ly/3LrmNQz
- Eisen GM, Baron TH, Dominitz JA, Faigel DO, Goldstein JL, et al. (2002) Guideline for the management of ingested foreign bodies. Gastrointest Endosc 55: 802–806. Link: https://bit.ly/36YhbON
- Mosca S, Manes G, Martino R, Amitrano L, Bottino V, et al. (2001) Endoscopic management of foreign bodies in the upper gastrointestinal tract: report on a series of 414 adult patients. Endoscopy 33: 692–696. Link: https://bit.ly/3uI86BY
- Ngan JH, Fok PJ, Lai EC, Branicki FJ, Wong J (1990) A prospective study on fish bone ingestion. Experience of 358 patients. Ann Surg 211: 459-462. Link: https://bit.ly/35hX1yy
- Zhang S, Cui Y, Gong X, Gu F, Chen M, et al. (2010) Endoscopic management of foreign bodies in the upper gastrointestinal tract in South China: a retrospective study of 561 cases. Dig Dis Sci 55: 1305-1312. Link: https://bit.ly/3iHxAK7
- Glaser J, Hack T, Rubsam M (1997) Unusual rectal foreign body: treatment using argon-beam coagulation. Endoscopy 29: 230–231. Link: https://bit.ly/3Nx3t60
- Billi P, Bassi M, Ferrara F, Biscardi A, Villani S, et al. (2010) Endoscopic removal of a large rectal foreign body using a large balloon dilator: report of a case and description of the technique. Endoscopy 42: E238. Link: https://bit.ly/3wLqvAj
- Saylir A, Duzgun IN, Guvendi B (2014) Treatment of unusual rectal foreign body using a Foley catheter. Endoscopy 46: E182–E183. Link: https://bit.ly/3uDXweT
- van der Wouden EJ, Westerveld D (2010) Extraction of a rectal foreign body using a custom-made giant snare. Endoscopy 42: E122. Link: https://bit.ly/3IO7eR1
- Yonem O, Ataseven H (2011) Endoscopic removal of iatrogenically induced rectal foreign body. Turk J Gastroenterol 22: 228–229. Link: https://bit.ly/3qIrkpE
- Yilmaz B, Ozmete S, Altimbas A, Aktas B, Ekiz F (2014) Successful removal of an unusual rectal foreign body with a Kocher clamp. Endoscopy 46: E549. Link: https://bit.ly/3Lewz8u
- Silva M, Albuquerque A, Ribeiro A, Cardoso H, Macedo G (2015) Ovbertube-guided endoscopic extraction of a rectal foreign body: lifting not only the embargo. Endoscopy 47: E563–E564. Link: https://bit.ly/3iQdn4x
- Lin XD, Wu GY, Li SH, Wen ZQ, Zhang F, et al. (2016) Removal of a large foreign body in the rectosigmoid colon by colonoscopy using gartrolith forceps. Worl J Clin Cases 4: 135–137. Link: https://bit.ly/3Lro36f
Article Alerts
Subscribe to our articles alerts and stay tuned.
 This work is licensed under a Creative Commons Attribution 4.0 International License.
This work is licensed under a Creative Commons Attribution 4.0 International License.




 Save to Mendeley
Save to Mendeley
