Journal of Surgery and Surgical Research
Long-term follow up of single-incision laparoscopic cholecystectomy compared to conventional laparoscopic cholecystectomy
Hayder Shabana1, Abdul-Karim Abbas2, Darragh Grace1, Jeremy Kay Hock Lee3* and Colm J O’Boyle1
2Sahlgrenska Academy, University of Gothenburg, Gothenburg, Sweden
3College of Medicine and Health, University College Cork, Ireland
Cite this as
Shabana H, Abbas AK, Grace D, Hock Lee JK, O’Boyle CJ (2020) Long-term follow up of single-incision laparoscopic cholecystectomy compared to conventional laparoscopic cholecystectomy. J Surg Surgical Res 6(1): 093-099. DOI: 10.17352/2455-2968.000105Purpose: Conventional Laparoscopic Cholecystectomy (CLC) is the “gold standard” approach for patients with gallstones. Single-incision Laparoscopic Cholecystectomy (SILC) was an alternative technique, purportedly offering several postoperative benefits over CLC. Studies comparing short-term postoperative outcomes of SILC versus CLC have yielded conflicting results. Our paper aims to compare the long-term postoperative outcomes of patients undergoing SILC and CLC with a minimum follow up of seven years.
Methods: A comparative retrospective study between SILC and CLC was conducted among 118 patients undergoing cholecystectomy from October 2008 to December 2010 (SILC=67/CLC=61). An initial retrospective chart review was performed. We later surveyed the patients who had undergone cholecystectomy by telephone interview at a mean(sd) of 4(0.75) years, and at 8(0.75) years. Postoperative outcomes were evaluated.
Results: No significant difference between SILC and CLC groups for daily pain scores (p = 0.45 and 0.97, for day 1 and 2, respectively), daily narcotic requirements (p = 0.09 and 0.85, for day 1 and 2, respectively), and time to return to normal activity (p = 0.11). The mean(sd) operative time was greater in SILC group [52(2.0) mins versus 36(2.3) mins; p <0.05]. There was a shorter mean(sd) length of stay postoperatively in the SILC group [2(0.11) days versus 3(0.32) days; p <0.05]. The SILC group had a higher median(sd) cosmetic satisfaction score (IQR) than the CLC group at both the intermediate-term [10(10) versus 9(8 to10); p <0.05] and long-term [10(10) versus 9(9to10); p <0.05] follow up.
Conclusion: SILC is associated with higher patient cosmetic satisfaction than CLC. However, the procedure is more technically challenging and associated with increased operating time and costs. The marginal cosmetic benefit at the expense of increased operative time and economic costs will likely mean that the choice of procedure will be largely patient rather than physician driven.
Introduction
The incidence of benign gallbladder disease has increased by more than 20% over the last four decades and affects over 15% of the adult population in the western world [1,2]. Laparoscopic cholecystectomy has been the “gold standard” approach for removal of the gallbladder. Conventional Laparoscopic Cholecystectomy (CLC) is performed by making several tiny incisions in the abdomen (Usually 4), allowing for the insertion of operating ports through which laparoscopic instruments can be introduced intra-abdominally. However, CLC has been associated with a wound infection rate of 1.3 to 3.5% and postoperative incisional site pain [3,4]. Surgeons have attempted to reduce the size, and/or number of incisions [4-7], in order to reduce wound infection rate and pain, and concurrently improve cosmesis [8].
In 1997, Navarra, et al. [6], performed the first SILC. This was achieved through a single incision at the umbilicus, thereby leaving a barely perceptible scar after the operation [9]. Numerous studies have shown that SILC offers better cosmesis, reduced postoperative pain, lesser complications and faster recovery time compared to CLC [4,10-12]. However, SILC has not gained widespread acceptance due to increased operative time (57.8mins versus 35.2mins), technical difficulty, minimal cosmetic benefit and analgesia benefit, and increased incisional hernia rates (13.3% versus 4.7%) [4,7,9,10,13-19]. The limitations of these studies were that the comparisons of postoperative outcomes between SILC and CLC were in the immediate postoperative period. These studies have yielded conflicting results and are thus inconclusive.
A more accurate approach would be to evaluate long-term outcomes, when the opportunity for improvements in the physical function, physical role, general health, and body pain are measurable; instead of focusing on each plausible outcome separately [7]. Furthermore, the evaluation of long-term cosmetic satisfaction is more credible compared to immediate cosmetic satisfaction following the surgery, where the incision has not been given sufficient time to fully heal [16]. Sato, et al. [20], have suggested that “studies of SILC performed by experienced surgeons with longer term follow up are necessary to determine the exact complication rate and profile.” Therefore, the aim of this study was to compare the long-term postoperative outcomes of patients undergoing SILC to a matched cohort of patients undergoing CLC with a minimum follow up of seven years.
Methods
Study design
This comparative retrospective study was conducted at the Department of Surgery, Bon Secours Hospital to evaluate long-term postoperative outcomes of SILC versus CLC, between October 2008 and December 2010, in patients presenting with symptomatic gallbladder disease. The study was conducted according to the principles of the Declaration of Helsinki and was approved by the ethical committee of Bons Secours Health System in Ireland.
Participants and data collection
Patients undergoing both elective and emergency cholecystectomy were included in the study. Exclusion criteria were: (a) previous multiple laparotomies, and/or (b) severe acute cholecystitis/empyema. Written informed consent was obtained from all the patients. Patients who had undergone SILC were also made aware that the conversion to CLC might be required if intraoperative difficulties were encountered.
Patients’ cosmetic satisfaction with the appearance of their scar(s) was assessed utilizing a standard Likert scoring system. Patients graded satisfaction on a scale of 1 to 10, with a higher score representing a greater satisfaction with the cosmetic result. Pain assessment of the port sites was assessed using a Visual Analog Scale (VAS). Patients placed a mark along a 10-cm vertical line, which denotes the severity of their pain, where “no pain” and “worst imaginable pain” were placed at the bottom and top of the line, respectively.
Short-term outcomes following the surgery were assessed during the hospital visit. A retrospective chart review was performed. Data on operative time, conversion rate, morbidity, analgesia requirements, postoperative pain score and duration of hospital stay was collected and analyzed. Patients were subsequently contacted by phone at 4(0.7) years after their procedures, to establish whether there was residual discomfort or any other previously undocumented complications remote from surgery. Enquiry was also made regarding time to return to normal activity and cosmetic satisfaction. These parameters were subsequently re-evaluated at 8(0.7) years after their procedures. This study is the longest follow-up for a comparative series of postoperative outcomes of SILC versus CLC reported in the literature.
Surgical access
All procedures were performed under general anesthesia. Antibiotics were prescribed only when intraperitoneal spillage of gallbladder contents occurred during laparoscopic cholecystectomy. Intraoperative analgesia included 6 mg of intravenous morphine with 75 mg of intramuscular diclofenac sodium, and 1g of intravenous paracetamol. Occasionally, 5mg of intravenous cyclomorphine was required in the recovery ward.
Conventional laparoscopic cholecystectomy
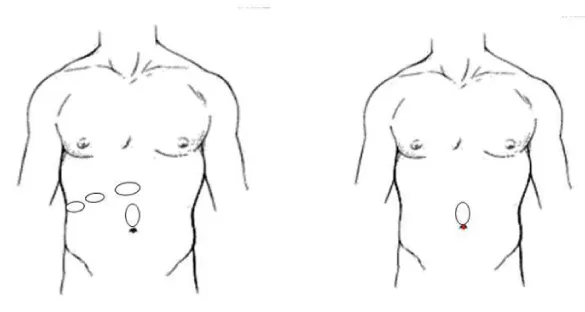
Under general anesthesia, the patient was placed in a supine position. After the patient was prepped and draped, pneumoperitoneum was created under direct vision by using a Hasson open technique 1 cm above the umbilicus (Figure 1a). An Ethicon 5-11 mm port was introduced, and a 12-15mmHg pneumoperitoneum was created. A 10 mm Laparoscopic Endo-eye (Olympus, Germany, WA50012A) was inserted through the port. After inspecting the abdomen, another three trocars were inserted under direct vision: (a) 12 mm port in the high epigastric region, (b) 5mm trocar at mid-axillary line halfway between the right costal margin and anterior superior iliac spine, and (c) 5mm port at the right midclavicular line just below the liver’s edge (Figure 1a). The gallbladder was dissected and placed in an endoscopic retrieval bag (Purple Surgical international limited, England) and removed via the epigastric incision. A PDS Ethicon (2/0) suture was utilized to close the fascia, and the skin was closed using Monocryl Ethicon (4/0) suture.
Single-Incision laparoscopic cholecystectomy
The patient was placed in a modified Lloyd-Davies position. The umbilicus was grasped at its base and everted utilizing two Littlewood forceps. A 1.5 cm skin incision was made within the umbilical fold (Figure 1b). A SILC port (Covedien, USA) was lubricated and introduced into the incision site and a 12-15mmHg pneumoperitoneum was created. A 5 mm Laparoscopic Endo-eye (Olympus, Germany, PI-0002229) and two trocars were placed through the SILC port. The patient was tilted to the left side and the gallbladder was sutured to the anterior abdominal wall by passing the suture through its fundus. The gallbladder was dissected in the standard fashion, placed in an endoscopic retrieval bag (Purple Surgical international limited, England), and removed via the central port site. A PDS Ethicon (2/0) suture was used to close the fascia, and the skin was closed using Monocryl Ethicon (4/0) suture.
Statistical analysis
Quantitative analysis, including mean ± Standard Deviation (SD) with 95% confidence intervals, median and Interquartile Range (IQR), was performed for the postoperative outcomes of patients in the SILC and CLC groups. The Student’s t test, including the Degrees of Freedom (df), were used to compare the means of both groups; whilst the Mann-Whitney U test was used to compare the medians of both groups (Where α = 0.05 is statistically significant). Non-parametric measure of the strength and direction of association that exists between age and cosmetic score was examined using Spearman’s correlation (r2). Learning curves were evaluated by the moving average method and cumulative sum (CUSUM) technique [21]. All statistical analyses were conducted using SPSS statistical software (version 17.0; SPSS, Inc., Chicago, IL, USA).
Results
A total of 118 patients were included in this study. There were 99 (83.9%) female and 19 (16.1%) male patients. The mean(sd) age of the patients in the CLC group was 53(12.9) years and of the SILC group was 45(12.0) years. 61(51.7%) patients underwent CLC whilst 57(48.3%) patients underwent SILC. All procedures were performed between October 2008 and December 2010. All CLC procedures were performed between October 2008 and April 2009. All SILC procedures were performed between July 2009 and December 2010. 10 patients (CLC=7/SILC=3) were lost to long-term follow-up.
A sub-analysis of the mean duration of operation in the SILC and CLC group was conducted. The mean(sd) duration of SILC operation in 2009 was not significantly different compared to 2010 [51.4(19.7) mins versus 52.5(11.0) mins; p= 4.28]. The mean(sd) duration of CLC operation for the first 9 cases was significantly different compared to the next 52 cases [65(28) mins versus 31.2(9) mins; p <0.05.
Patient demographics and clinical characteristics
Patient demographics are shown in Table 1. The proportion of female patients in the CLC and SILC groups were 80% and 89% respectively. There was no significant difference between the two groups of patients for sex (p = 0.11). The mean(sd) Body Mass Index (BMI) was higher in the CLC group [28(6) kg/m2 versus 25(6) kg/m2; p<0.05, 95% CI (1.465, 5.699)]. The mean(sd) age of the CLC group was also higher [53(12.9) years versus 45(12.0) years; p <0.05, 95% CI (3.636, 12.882)].
Clinical characteristics are presented in Tables 2,3 3. 21% of patients in the CLC group had acute cholecystitis compared to 12% of patients in the SILC. This difference was not statically significant [p = 0.4; p = 0.39, 95% CI (-0.30, 0.12)] (Table 2). The mean(sd) length of postoperative stay in the CLC group was higher [3(0.32) days versus 2(0.11) days; p <0.05, 95% CI (0.14, 1.858)] (Table 2). However, the mean(sd) procedure duration was longer for the SILC group [52(2.3) mins versus 35(2.0) mins; p <0.05, 95% CI (-17.788, -16.212)] (Table 2).
The median postoperative pain score [IQR] between CLC and SILC groups was similar at day 1 [7 (5.5 to 8) vs. 7 (7 to 8); p =0.45] and day 2 [4 (3 to 7) vs. 4 (3 to 6); p =0.97] (Table 3). Furthermore, no significant difference was observed between CLC and SILC groups for median narcotic doses at both day 1 (100mg vs 0mg; p = 0.09) and day 2 (100mg vs 100mg; p = 0.84), (Table 3).
Learning curves
No significant complications occurred for both SILC and CLC groups intraoperatively and no procedure required a laparotomy. However, two (3.5%) patients undergoing SILC required the insertion of an additional 5 mm port due to technical difficulties.
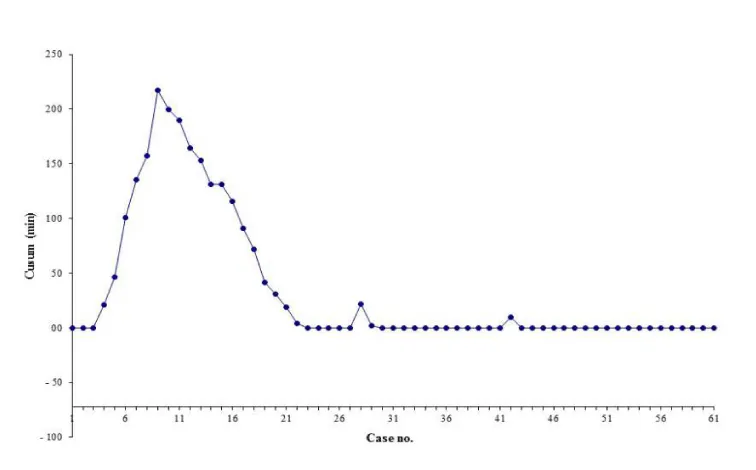
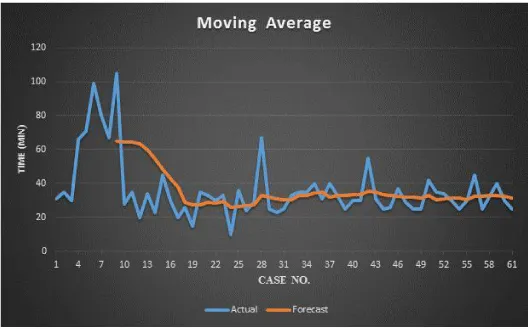
Analysis of learning curves for operating times of both procedures was performed using Cumulative Sum control chart (CUSUM) and moving average method [21]. This was to assess if either technique was associated with a change in procedure duration over time.
Figure 2 depicts the overall learning curve for CLC patients, showing one peak at the 9th case. The mean surgery duration in CLC for the first 9 cases [t(59) = 6.9, p<0.05, 95% CI (23.96, 43.3); Table 4]. The overall trend for surgery duration in CLC calculated using the moving average method revealed an abrupt decrease after the 9th case (Figure 3).
On the other hand, the learning curve for overall SILC patients by one surgeon reveals no indication of a change in the process mean [51.4(19.7) mins versus 52.5(11.0) mins; p = 4.28]. This is further confirmed by the moving average method showing a stable trend for operative time in SILC [65(28) mins versus 31.2(9) mins; p <0.05].
Cosmetic satisfaction
The mean(sd) age of SILC group is lower than the CLC group [45(12.0) years versus 53(12.9) years; p=0.01] (Table 1). We plotted age vs cosmetic scores at intermediate and long-term follow up phases and examined the correlation coefficient of the variables. At intermediate-term follow up at 4(0.75) years, neither CLC nor SILC patients showed significant correlation between the score and age (r2 = 0.17, p = 0.17, and r2 = 0.01, p = 0.92, for CLC and SILC groups, respectively). However, at the long-term follow up phase at 8(0.75) years, only CLC patients revealed significant but weak positive correlation between their age and scores (r2 = 0.3, p <0.05, and r2 = 0.01, p = 0.95, for CLC and SILC groups, respectively).
Intermediate-term follow-up
61 patients (100%) in the CLC group and 56 patients (98%) in the SILC group were contactable at 4(0.75) years. There was no significant difference in median (IQR) number of days to return to work for CLC group compared to SILC group [14(14-21) days versus 14 (14-21) days; U = 1458.5; p = 0.11] (Table 5). However, the median cosmetic score (IQR) was higher for SILC group [10(10) versus 9(8-10); U = 752.5; p <0.05] (Table 6). One patient in the SILC group (1.7%) developed a trocar-site hernia after two years from the operation (U = 1677.5; p = 0.29). No other complications were reported in either group.
Long-term follow-up
54 patients (89%) in the CLC group and 54 patients (95%) in the SILC group were contactable at 8(0.75) years following surgery. The median cosmetic scores (IQR) was again higher for SILC group [10(10) versus 9(9-10); U = 971; p <0.05] (Table 6). No other postoperative life threatening or permanently disabling complications was reported in either group of patients.
Discussion
Numerous studies have shown that SILC is associated with better cosmesis, reduced pain, and quicker recovery [4,10-12]. However, SILC has not gained widespread acceptance possibly because it is a more technically challenging operation than CLC [7,22]. Additionally, SILC has been associated with longer procedure times and more complications, without significant benefit in terms of patients’ satisfaction, postoperative pain, and quality of life [7,19,22]. This was likely attributed to the technical difficulties faced during the procedure which include instrument clashing, reduced visibility, and reduced mobility of instruments. More recently, more SILC-specific instrumentation has been developed. However, we report a higher mean surgery duration for SILC of 52 ± 2 mins, compared to the experiences reported from several studies [4,14,23-26]. Postoperative pain, use of an additional port, complication rates, operation time and the costs of SILC were similar to or greater than those of CLC [27]. Hence, large randomized controlled trials are needed to examine the true benefits of SILC.
Studies have demonstrated that a reduction in the size and/or number of ports in SILC resulted in decreased postoperative pain [5,17,28] and analgesic requirements compared to CLC [5,28]. However, we failed to demonstrate any significant differences in terms of overall pain scores or analgesic requirements between both groups. These findings were consistent with other series reported in the literature [14,16,26]. While there has been a reduction in the number of 5mm ports utilized in SILC; the umbilical incision in SILC however is invariably larger than in CLC. We believe that this is the principal determinant in the lack of significant benefit in terms pain for SILC [28,29]. However, in our study, the post operative hospital stay in SILC arm is less than that of CLC group which was statistically significant (P<0.05) and the pain is one of the main reason for staying longer in the hospital [30].
We were initially concerned that a larger umbilical incision in the SILC group was the possibility of a higher incidence of umbilical hernias [31-33]. A number of studies did not detect any port site hernia or wound complications [4,5,14]. However, the follow up periods for these studies were less than 12 months which would likely underestimate the incidence. Despite these concerns, we did not detect any significant differences at long-term follow up intervals.
There was no significant improvement in operating time for SILC throughout our series, which was consistent with previous reports [4,10,17,23-26]. This suggests that surgeons experienced with laparoscopic cholecystectomy can transfer to a single incision laparoscopic cholecystectomy relatively easily but that improvement in operative time with increased experience was due to technical/instrumentation difficulty.
Although SILC is safe and effective, inherent surgeons’ discomfort prevented a large-scale adaption of this technique. Recent advances in robotic technology suggests that da Vinci Single-SiteTM cholecystectomy (dVSSC) may overcome this issue(33). dVSSC provides significant benefits over SILC in terms of surgeon’s stress load, matches the standards of single incision approach with regard to patients’ outcomes but increases expenses.
Conclusion
We found SILC to be a safe procedure, without significant increase in morbidity compared to CLC. The improved cosmetic satisfaction with SILC persisted at intermediate and long-term follow up. However, SILC is associated with longer operative times and greater costs compared to CLC. Somewhat surprisingly, we did not find any benefit in terms of postoperative analgesic requirements and return to normal activity. We are cautiously optimistic that with improved instrumentation, SILC will become more commonplace in the future. However, the marginal cosmetic benefit at the cost of increased operative time and costs will likely mean that the choice of the procedure will be largely patient rather than physician driven.
Author contributions
Substantial contributions to the conception or design of the work: Colm J O’Boyle.
Acquisition, analysis, or interpretation of data for the work: Hayder Shabana, Abdul-Karim Abbas, Darragh Grace and Jeremy Kay Hock Lee. Drafting the work or revising it critically for important intellectual content: All authors, listed under the title of the article.
Final approval of the version to be published: All authors, listed under the title of the article.
Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved: All authors, listed under the title of the article.
- Shaffer EA (2005) Epidemiology and risk factors for gallstone disease: Has the paradigm changed in the 21st century? Curr Gastroenterol Rep 7: 132-140. Link: https://bit.ly/38bjIlh
- Stinton LM, Shaffer EA (2012) Epidemiology of gallbladder disease: cholelithiasis and cancer. Gut Liver 6: 172-187. Link: https://bit.ly/389FDJr
- Velanovich V, Morton JM, McDonald M, Orlando R, Maupin G, et al. (2006) Analysis of the SAGES outcomes initiative cholecystectomy registry. Surg Endosc 20: 43–50. Link: https://bit.ly/2NFLfBU
- Khorgami Z, Shoar S, Anbara T, Soroush A, Nasiri S, et al. (2014) A Randomized Clinical Trial Comparing 4-Port, 3-Port, and Single-Incision Laparoscopic Cholecystectomy. J Invest Surg 27: 147-154. Link: https://bit.ly/3dFmPTl
- Oruc MT, Ugurlu MU (2013) Extraumbilical Single-Incision Laparoscopic Cholecystectomy with Standard Laparoscopic Instruments. Scand J Surg 102: 209-214. Link: https://bit.ly/3g1OKhY
- Navarra G, Pozza E, Occhionorelli S, Carcoforo P, Donini I (1997) One-wound laparoscopic cholecystectomy. Br J Surg 84: 695. Link: https://bit.ly/31okXfq
- Sulu B, Yildiz B, Ilingi E, Gunerhan Y, Cakmur H, et al. (2015) Single Port vs. Four Port Cholecystectomy– Randomized Trial on Quality of Life. Adv Clin Exp Med 24: 469-473. Link: https://bit.ly/3eHET0L
- Qu JW, Xin C, Wang GY, Yuan ZQ, Li KW (2019) Feasibility and safety of single-incision laparoscopic cholecystectomy versus conventional laparoscopic cholecystectomy in an ambulatory setting. Hepatobiliary Pancreat Dis Int 18: 273-277. Link: https://bit.ly/38aDr4h
- Arezzo A, Passera R, Forcignanò E, Rapetti L, Cirocchi R, et al. (2018) Single-incision laparoscopic cholecystectomy is responsible for increased adverse events: results of a meta-analysis of randomized controlled trials. Surg Endosc 32: 3739–3753. Link: https://bit.ly/31ssc62
- Tsimoyiannis EC, Tsimogiannis KE, Pappas-gogos G, Farantos C, Benetatos N, et al. (2010) Different pain scores in single transumbilical incision laparoscopic cholecystectomy versus classic laparoscopic cholecystectomy: a randomized controlled trial. Surg Endosc 24: 1842-1848. Link: https://bit.ly/3ibRDyQ
- Lirici MM, Tierno SM, Ponzano C (2016) Single-incision laparoscopic cholecystectomy: does it work? A systematic review. Surg Endosc 30: 4389-4399. Link: https://bit.ly/2NJGpDn
- Haueter R, Schütz T, Raptis DA, Clavien PA, Zuber M (2017) Meta-analysis of single-port versus conventional laparoscopic cholecystectomy comparing body image and cosmesis. Br J Surg 104: 1141-1159. Link: https://bit.ly/2AaHqkO
- Gaillard M, Tranchart H, Lainas P, Dagher I (2015) New minimally invasive approaches for cholecystectomy: Review of literature. World J Gastrointest Surg 7: 243-248. Link: https://bit.ly/2YEHsLf
- Arezzo A, Passera R, Bullano A, Mintz Y, Kedar A, et al. (2017) Multi-port versus single-port cholecystectomy: results of a multi-centre, randomised controlled trial (MUSIC trial). Surgical Endoscopy New York 31: 2872-2880. Link: https://bit.ly/2ND2Qdt
- Phillips MS, Marks JM, Roberts K, Tacchino R, Onders R, et al. (2012) Intermediate results of a prospective randomized controlled trial of traditional four-port laparoscopic cholecystectomy versus single-incision laparoscopic cholecystectomy. Surg Endosc 26: 1296-1303. Link: https://bit.ly/2BbIXYF
- Saad S, Strassel V, Sauerland S (2013) Randomized clinical trial of single-port, minilaparoscopic and conventional laparoscopic cholecystectomy. Br J Surg 100: 339-349. Link: https://bit.ly/2Zgye7b
- Zheng M, Qin M, Zhao H (2012) Laparoendoscopic single-site cholecystectomy: A randomized controlled study. Minim Invasive Ther Allied Technol 21: 113-117. Link: https://bit.ly/31rIZpK
- Hoyuela C, Juvany M, Guillaumes S, Ardid J, Trias M, et al. (2019) Long-term incisional hernia rate after single-incision laparoscopic cholecystectomy is significantly higher than that after standard three-port laparoscopy: a cohort study. Hernia 23: 1205-1213. Link: https://bit.ly/2VnbjWD
- Ito E, Takai A, Imai Y, Otani H, Onishi Y, et al. (2019) Quality of life after single-incision laparoscopic cholecystectomy: A randomized, clinical trial. Surgery 165: 353–359. Link: https://bit.ly/38aeiXp
- Sato N, Shibao K, Mori Y, Higure A, Yamaguchi K (2015) Postoperative complications following single-incision laparoscopic cholecystectomy: a retrospective analysis in 360 consecutive patients. Surg Endosc 29: 708-713. Link: https://bit.ly/2Znox6K
- Kim CW, Lee KY, Lee SC, Lee S-H, Lee YS, et al. (2017) Learning curve for single-port laparoscopic colon cancer resection: a multicenter observational study. Surg Endosc 31: 1828-1835. Link: https://bit.ly/2BSJNJt
- Omar MA, Redwan AA, Mahmoud AG (2017) Single-incision versus 3-port laparoscopic cholecystectomy in symptomatic gallstones: A prospective randomized study. Surgery 162: 96–103. Link: https://bit.ly/2YH7iOL
- Borle FR, Mehra B, Ranjan Singh A (2015) Comparison of Cosmetic Outcome Between Single-Incision Laparoscopic Cholecystectomy and Conventional Laparoscopic Cholecystectomy in Rural Indian Population: A Randomized Clinical Trial. Indian J Surg 77: 877-880. Link: https://bit.ly/3eIDSVT
- Justo-Janeiro JM, Vincent GT, Vázquez de Lara F, de la Rosa Paredes R, Orozco EP, et al. (2014) One, Two, or Three Ports in Laparoscopic Cholecystectomy? Int Surg 99: 739-744. Link: https://bit.ly/2ZnoWGi
- Lee CJ, Clark JM, Schweitzer M, Magnuson T, Steele K, et al. (2015) Prevalence of and risk factors for hypoglycemic symptoms after gastric bypass and sleeve gastrectomy. Obesity (Silver Spring) 23: 1079-1084. Link: https://bit.ly/3i9kH9X
- Zapf M, Yetasook A, Leung D, Salabat R, Denham W, et al. (2013) Single-incision results in similar pain and quality of life scores compared with multi-incision laparoscopic cholecystectomy: A blinded prospective randomized trial of 100 patients. Surgery 154: 662-671. Link: https://bit.ly/2CIZYJQ
- Lee SR, Kim HO, Shin JH (2019) Clinical outcomes of single-incision robotic cholecystectomy versus conventional 3-port laparoscopic cholecystectomy. Can J Surg 62: 52-56. Link: https://bit.ly/2Zkd4Vv
- Asakuma M, Hayashi M, Komeda K, Shimizu T, Hirokawa F, et al. (2011) Impact of single-port cholecystectomy on postoperative pain. BJS (British Journal of Surgery) 98: 991-995. Link: https://bit.ly/38bJNAy
- Gurusamy KS, Vaughan J, Rossi M, Davidson BR (2014) Fewer‐than‐four ports versus four ports for laparoscopic cholecystectomy. Cochrane Database of Systematic Reviews. Link: https://bit.ly/3eIgUOT
- Lau H, Brooks DC (2001) Predictive Factors for Unanticipated Admissions After Ambulatory Laparoscopic Cholecystectomy. Arch Surg 136: 1150-1153. Link: https://bit.ly/2ZmVUqB
- Milas M, Deveđija S, Trkulja V (2014) Single incision versus standard multiport laparoscopic cholecystectomy: Up-dated systematic review and meta-analysis of randomized trials. Surgeon 12: 271-289. Link: https://bit.ly/3g8MLIW
- Alptekin H, Yilmaz H, Acar F, Kafali ME, Sahin M (2012) Incisional hernia rate may increase after single-port cholecystectomy. J Laparoendosc Adv Surg Tech A 22: 731-737. Link: https://bit.ly/3ic2Orb
- Grochola LF, Soll C, Zehnder A, Wyss R, Herzog P, et al. (2019) Robot-assisted versus laparoscopic single-incision cholecystectomy: results of a randomized controlled trial. Surg Endosc33: 1482–1490. Link: https://bit.ly/2BRkBmY
Article Alerts
Subscribe to our articles alerts and stay tuned.
 This work is licensed under a Creative Commons Attribution 4.0 International License.
This work is licensed under a Creative Commons Attribution 4.0 International License.

 Save to Mendeley
Save to Mendeley
