Journal of Surgery and Surgical Research
Omental Cyst: An Atypical Presentation in a Child Masquerading Tubercular Ascites with Severe Acute Malnutrition and Sickle Cell Disease
Samarth Gupta*
Cite this as
Gupta S (2017) Omental Cyst: An Atypical Presentation in a Child Masquerading Tubercular Ascites with Severe Acute Malnutrition and Sickle Cell Disease. J Surg Surgical Res 3(1): 006-009. DOI: 10.17352/2455-2968.000035Introduction: Omental cysts are rare abdominal lesions which may be difficult to diagnose. The incidence of cystic lesions is about 1 per 140,000 general hospital admissions and about 1 per 20,000 pediatric hospital admissions. Most common presentation is abdominal distension. However, they may be an incidental finding or a painless abdominal mass and often mimicking ascites. The presentation is confusing in some cases which may result in mismanagement, added costs and trouble to the patient.
Case Report: Here we encountered a case of a large omental cyst which was initially treated as tubercular peritonitis with ascites. The patient also suffered from malnutrition and was diagnosed a case of sickle cell disease adding to the dilemma in the final diagnosis. The USG report also suggested tubercular peritonitis with gross ascites. However, the CT scan suggested of omental cyst which was confirmed intra operatively and on histopathological examination. The cyst was successfully removed and the patient was discharged.
Conclusion: Children presenting with abdominal distension should be carefully investigated to get to the correct diagnosis due to paucity of definitive signs and symptoms especially in omental cysts. Despite of all the investigations, the diagnosis may still be a dilemma. USG and CT is keystone in the diagnosis. Finally, once diagnosed an omental cyst can be safely removed.
Introduction
Omental Cysts are rare intra-abdominal lesions that are found in children. The incidence of cystic lesions is about 1 per 140,000 general hospital admissions and about 1 per 20,000 pediatric hospital admissions. They are far less common than mesenteric cysts. They may present as an asymptomatic abdominal mass or may cause abdominal pain with or without appreciable mass or distension. Physical examination may reveal a freely mobile intra-abdominal mass. Both CT and abdominal ultrasound reveal a well circumscribed cystic mass lesion arising from greater omentum. Treatment involves resection of all symptomatic omental cysts. Here in this case the patient came with complaints of abdominal distension with features of severe malnutrition. She also turned out to be sickle positive making the diagnosis a dilemma. Further ultrasound report was suggestive of sclerosing peritonitis and the patient was started on AKT. Fluid aspirate results further made confusion in the diagnosis. It was only on CT scan that an omental cyst was put into the diagnosis. The patient underwent laparotomy and the cyst was safely removed. It is therefore important to adequately investigate a patient presenting with such features and thereby keeping omental cyst as a differential in our minds.
Case Report
A 4 year old female child presented with complaints of abdominal distension since 1 month, breathlessness on exertion (NYHA grade 2) since 1 month, reduced urine output since 1 month, pedal edema since 15 days, fever since 15 days. She had a normal birth history with full term normal delivery at home with no immunization status. Patient had features of acute malnutrition having moderate stunting although the weight: height ratio seemed within normal limits. On examination, patient was irritable, tachycardic, pallor: present, abdomen: distended, tender, shifting dullness: absent, fluid thrill: present. No signs of respiratory distress.
Laboratory Investigations revealed Hb: 7.9, Total count of 10600, Differential Count: 56 neutrophils and 41 lymphocytes, ESR: 14, Reticulocyte count: 6.0, Sickeling test positive, Hb electrophoresis revealing Sickle Cell disease in this patient.
Abdominal Sonography finding: Gross free fluid in abdominal cavity with internal echoes and separations pushing bowels posteriorly finding suggestive of Sclerosing peritonitis/Abdominal cocoon and an associated mild splenomegaly.
Fluid Examination had the following findings
Protein: 3.2 gm/dl, glucose: 74
WBC: 420/cc; Polymorphs: 5%; Lymphocytes 95%
ADA: 35.22 Gene Xpert: negative
Anti-tubercular therapy was started considering the sonographical findings and fluid aspirate examination.
Discussion
The patient was admitted in pediatrics ward for abdominal distension and fever. Abdominal sonography, fluid tap investigations namely the lymphocyte count led the pediatricians to start anti tubercular therapy. However, the CT scan report revealed the presence of an Omental Cyst, after which the patient was transferred to Surgery ward. The patient was not in sickle crises at this time.
Omental Cysts are rare abdominal lesions. The incidence is about 1 per 140,000 general hospital admissions and about 1 per 20,000 pediatric hospital admissions [1]. Mean age of children affected is 4.9 years.
They are thought to represent benign proliferations of ectopic lymphatics that lack communication with the normal lymphatic system. Cysts are thought to arise from lymphatic spaces associated with the embryonic retroperitoneal lymph sac [2].
Other etiological theories: Failure of leaves of mesentry to fuse, failure of embryonic lymph nodes to fuse, trauma, neoplasia, degeneration of Lymph nodes.
Omental cysts are confined to the greater or lesser omentum. Most common site is greater omentum. Omental cyst presents mostly with abdominal distension but they may be discovered as an incidental finding during laparotomy for another condition, or it may manifest as an acute abdomen [3]. Omental cysts may be a result of demoid cysts [4], or teratomas [5]. Omental cysts can be either simple or multiple and either unilocular or multilocular, and may contain hemorrhagic, serous, chylous, or infected fluid [2]. Fluid is serous in ileal and chylous in jejunal cysts [6]. In this case the patient did present with distension and abdominal pain however, the chief complaints also included fever, decreased urine output, pedal edema. The mass was indeed large, and simulated ascites.
After ruling out other causes for edema such as nephrotic syndrome, they came to the conclusion that the edema may have corresponded to malnutrition which was supplemented by clinical and laboratory investigations. The patient was anemic and a sickle profile was conducted as the patient belonged from the sickle belt, which turned out to be positive. However, it was more of an incidental finding as the peripheral smear also consisted of target cells and ovalocytes suggesting nutritional and B12 deficiency anemia.
The fluid aspirate showed a raised count which consisted of lymphocytosis. All this and the abdominal sonographical report prompted the pediatrician to start Anti Tubercular therapy.
Various complications have been associated with mesenteric and omental cysts, including the following: [3]
• Intestinal obstruction (most common)
• Volvulus
• Hemorrhage into the cyst
• Infection
• Rupture
• Cystic torsion
• Obstruction of the urinary and biliary tract
Radiography
Plain abdominal radiography may reveal a gasless, homogeneous, water-dense mass that displaces bowel loops posteriorly in the presence of an omental cyst.
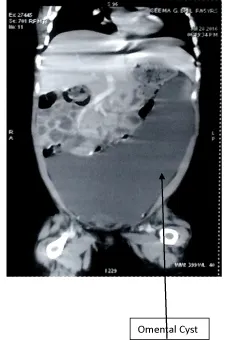
Computed tomography
Well defined thin wall enhancing cystic lesion measuring 20x15 cm seen in abdomen and pelvis on left side probably involving omentum. Small bowel loops displaced to right. The lesion was indenting on stomach, descending, transverse and sigmoid colon. The lesion was abutting anterior abdominal wall on both sides. Internal septations seen p/o Benign Cyst (Figure 1).
Approach
No medical therapy is available. In children with mesenteric or omental cysts, the most common indication for surgical intervention is the presence of an abdominal mass with or without signs of intestinal obstruction.
Surgery
The goal of surgical therapy for mesenteric and omental cysts is complete excision of the mass. Omental cysts can be removed without endangering the adjacent bowel. If enucleation or resection is not possible because of the size of the cyst or because of its location deep within the root of the mesentery, the third option is partial excision with marsupialization of the remaining cyst into the abdominal cavity. Approximately 10% of patients require this form of therapy. If marsupialization is performed, the cyst lining should be sclerosed with 10% glucose solution, ]electrocautery, or tincture of iodine to minimize recurrence. Partial excision alone with or without drainage is not indicated because of the high recurrence rate associated with these procedures.
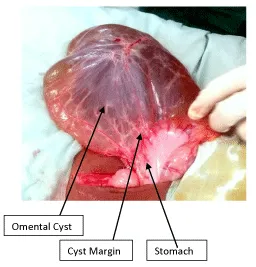
Laparoscopic management of mesenteric cysts is also being reported. If necessary, depending on the expertise in laparoscopic surgery in children, laparoscopy could be used to localize the cysts, and resection could be performed through a small laparotomy or via an extended umbilical incision (Figure 2).
Procedure
The patient underwent standard preoperative care, which included improving the Hb status. After fitness from pediatrician the patient was taken for surgery. Nasogastric tube insertion, preop antibiotic dose was given. A midline laparotomy incision was taken and cyst was found to be arising from greater omentum extending from stomach to transverse colon. A part of it was adhered to small bowel but did not seem to arise from it. Whole of the cyst was removed in toto.
Postoperative notes
After operative treatment, the patient was maintained on NPO (nil per oral) status with IV fluids and nasogastric suction until bowel function returned. Antibiotics were continued and the patient was started on fluids on the 3rd post op day. The patient did well and was discharged after her sutures were removed.
Histological findings
Classification of mesenteric and omental cysts in our study histopathologically according to updated classification recommended by Marc de Perrot [3] [7].
Non-Pancreatic Pseudocysts (Most common)
Simple lymphatic cyst (chylous cyst, lymphocele)
Lymphangioma
Enteric duplicationCyst
Enteric cyst
Embryonic vestigial
Urogenital cyst
Mature cystic
Teratomas
The section from this cyst wall showed lining by flat cuboidal cells. The wall showed fibrocollagenous tissue with congested blood vessels with, areas of haemorrhage and lymphoid aggregates- Benign serous cyst.
Conclusion
Omental cysts are rare abdominal lesions and may present with a variety of complaints. Due to this there may be a misdiagnosis and this would result in added costs and trouble to the patient. Therefore, it is important for the clinician to adequately investigate the patient in order to prevent such happenings. An ultrasound and CT is the keystone in the diagnosis of an omental cyst. However, one should be careful to identify complications of omental cysts.
- Kurtz RJ, Heimann TM, Holt J, Beck AR (1986) Mesentric and retroperitoneal cysts. Ann Surg 203: 109-112. Link: https://goo.gl/wQUBCl
- Egozi EI, Ricketts RR (1997) Mesenteric and omental cysts in children. Am Surg 63: 287-290. Link: https://goo.gl/OlhO5m
- Ricketts RR (1998) Mesentric and omental cysts. Pediatric Surgery. 5th ed. 1269-1275. Link: https://goo.gl/qGjIuE
- Schols RM, Stassen LP, Keymeulen KB, Bouvy ND (2012) Dermoid cyst of greater omentum teratoma. Srp Arh Celok Lek 140: 362-364.
- Sforza M, Andjelkov K, Ivanov D, Maricic Z, Krstic S (2012) A rare case of omentum teratoma. Srp Arh Celok Lek 140: 362-364. Link: https://goo.gl/rKvR7W
- Vanek VW, Phillips AK (1984) Retroperitoneal, mesenteric and omental cysts. Arch Surg. Jul. 119: 838-842. Link: https://goo.gl/y5zIRQ
- M Ramani, Kazi Wajid Husain, OH Radhika Krishna, Ramesh Reddy, P Sreenivasa Reddy, et al. (2013) Histopathological Review of mesenteric and omental Cysts in children. JEMDS 2: 4701-4709. Link: https://goo.gl/wxxDR4
- Neal E Seymour; Robert L Bell (2015) Schwartz’s principles of surgery. Abdominal wall, omentum, mesentry and retroperitoneum. 35: 1457. Link: https://goo.gl/b3RVNG
- Beahrs OH, Judd ES, Dockerty MB (1953) Chylous cysts. Philadelphia, Pa: WB Saunders Co 377.
Article Alerts
Subscribe to our articles alerts and stay tuned.
 This work is licensed under a Creative Commons Attribution 4.0 International License.
This work is licensed under a Creative Commons Attribution 4.0 International License.

 Save to Mendeley
Save to Mendeley
