Journal of Surgery and Surgical Research
Treatment of chronic instability of the patella by ligamentoplasty of the medial patellofemoral ligament
MJEL Mekkaoui, HEl Ouagari*, M Boufettal, RA Bassir, M Kharmaz, MO Lamrani and MS Berrada
Cite this as
Mekkaoui MJEL, Ouagari HEl, Boufettal M, Bassir RA, Kharmaz M, et al. (2024) Treatment of chronic instability of the patella by ligamentoplasty of the medial patellofemoral ligament. J Surg Surgical Res 10(1): 022-026. DOI: 10.17352/2455-2968.000162Copyright
© 2024 Mekkaoui MJEL, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.Objective and potential Patellofemoral Instability (PFI) is linked to different anatomical anomalies.
It has been suggested that in the majority of cases of patellar dislocation, the Medial Patellofemoral Ligament (MPFL) is ruptured with a high recurrence rate, particularly in female patients. Although MPFL tear is not the primary cause of instability, MPFL reconstruction is effective in stabilizing the knee and can single-handedly prevent lateral patellar dislocation. There is limited but growing evidence that MPFL reconstruction for patellofemoral instability leads to excellent functional outcomes.
In this work, we report our technique of MPFL reconstruction using the gracilis tendon with a review of recent literature concerning MPFL reconstruction and functional results in the face of objective patellar instabilities treated solely by MPFL reconstruction.
Introduction
Acute patellar dislocation is primarily an injury affecting young, active patients of both sexes, with a higher recurrence rate in female patients. The overall recurrence rate after primary patellar dislocation approaches 40%. Patients with primary patellar dislocation have a recurrence rate of 17% and patients with repeated patellofemoral dislocation have a recurrence rate of 49% [1,2].
Chronic patellar instability is a condition where the patella bone pathologically disarticulates out from the patellofemoral joint, either subluxation or complete dislocation. This most often involves multiple factors. Patients with patellar instability can have debilitating pain, limitations in basic function, and long-term arthritis [3,4].
There is growing interest in the soft tissue structure that helps stabilize the patella. Medial Patellofemoral Ligament (MPFL) deficiency is reported to be 50% to 96% in those who suffered traumatic patellar dislocation during open surgical exploration. A rupture of this structure always occurs during a lateral patellar dislocation because the MPFL can undergo a maximum elongation of 20% to 30% (extremes: 18 mm to 20 mm); this is much less than the patellar width, which often exceeds 40 mm [5,6].
The MPFL is often damaged during patellar subluxation or dislocation and, therefore, over the past decade, several authors have recommended repair or reconstruction of the MPFL to reduce the high incidence of recurrent dislocation, and numerous surgical techniques for reconstruction or repair of the MPFL have been described. The purpose of this article is to demonstrate that MPFL reconstruction is effective in stabilizing the knee and can single-handedly prevent lateral patellar dislocation. The techniques are multiple, respecting the anchoring points on the patella and the medial femoral condyle as well as adjusting the tension of the ligamentoplasty are the guarantees of a good result [7-9].
Observation
This is a 19-year-old patient who presented with patellar instability following three episodes of dislocation of the left patella, the first episode of which dates back 3 years. All three reduced spontaneously.
The patient was followed in pediatrics for 1 year and then was referred to us when she turned 18.
The clinical examination reveals hyperlaxity of the patella, a varus morphotype of the knees, no pain on palpation, and an audible crack during flexion-extension of the left knee in connection with patellofemoral dysplasia increased by the deficit of the medial ligament plane (Figure 1).
No clinical signs of associated meniscus or ligamentous lesions on MRI.
Standard frontal and lateral X-rays as well as axial views of 30, 60, and 90 degrees were requested and the first consultation (Figure 2a,2b). They showed subluxation of the patella, tearing of the internal patellar wing, and external patellofemoral narrowing with a CATON-DESCHAMPS INDEX of 1.3 (Patella Alta).
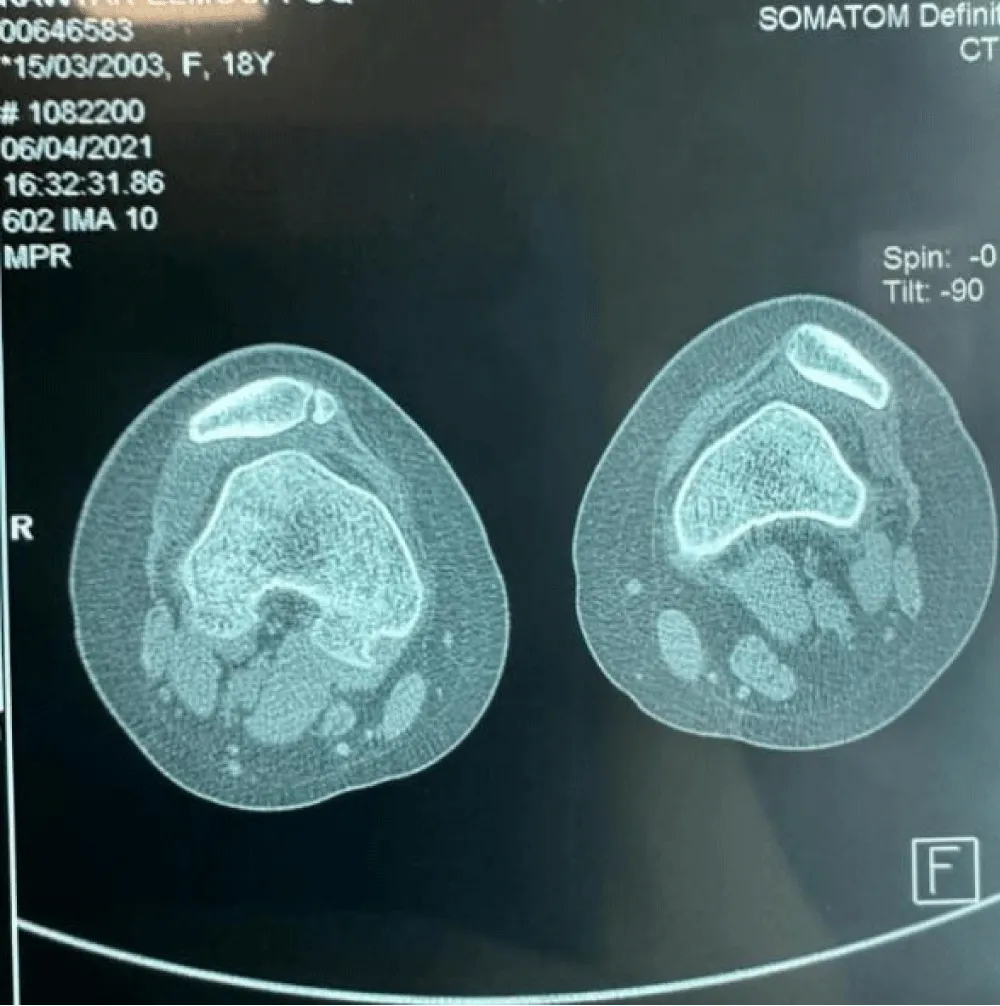
The CT scan (Figure 3) of the knee revealed a slightly elevated TAGT (anterior tuberosity – trochlear throat distance) on the left side.
Left: TAGT in flexion = 12 mm
TAGT in extension = 22 mm
Right: TAGT in flexion = 12 mm
TAGT in extension = 20 mm
With respect to the bony cortices, the patellofemoral joint, and the peri-articular soft parts of the knee.
The diagnosis of trochlear dysplasia type A and patellar instability was made.
Surgical technique
Our patient benefited from ligamentoplasty of the MPFL using the Gracilis tendon.
An incision next to the crow's feet tendonitis was made, followed by removal of the gracilis tendon using a stripper and cleaning of the latter of its muscle fibers.
A second 3cm internal parapatellar incision was made followed by trans-osseous tunneling of the patella at the level of the upper half of the medial bank of the patella and passage of the prepared tendon through 2 tunnels joined together in the form of “V”.
The 2 strands of the tendon were recovered, threaded, and secured at their ends, leaving a traction wire (Figure 4). A long Halshted forceps was passed under the internal retinaculum of the knee but extra synovial and retrieved approximately 1 cm below and in front of the medial epicondyle.
Creation of a tunnel at the level of the femoral insertion 11mm behind and above the medial epicondyle and 11mm in front and below the adductor tubercle and fixation of the graft with 7 mm interference screw between 20 and 30 degrees of flexion of the knee after adjusting the tension which should leave an external translation play of the patella of 6 to 8 mm (Figure 5).
Results
The postoperative period was simple with passive mobilization of the knee the next day, walking with support protected by two canes, and a knee brace also the next day. the knee brace was kept for 6 weeks with passive mobilization, with a presentor, and with arthromotor authorized from the first week. Muscular awakening with electro stimulation was started the next day, and muscle strengthening after 2 weeks.
After a follow-up of 18 months in this patient and an average follow-up of 20 months in all of our patients operated by the same technique (5 patients), we note a significant functional improvement without any case of recurrence of the dislocation, the sign of ‘Smilie’ disappeared in all patients, the axial radiographs compared to the contralateral knee show an improvement in the centering of the patella (Figure 6).
Discussion
MPFL injury occurs at a rate between 94 and 100% following patellar dislocation. Traumatic lesions of this ligament, if not treated, can lead to recurrent dislocations in 14 to 44% of cases, osteochondral lesions, and ultimately, early osteoarthritis. In order to avoid any future complications, surgical intervention to restore normal anatomy is mandatory due to the high risks of experiencing more recurring dislocation episodes compared to conservative treatments of any kind [1,10].
According to the latest studies, the difference between non-operative and operative treatment lies not in the functional scores, which are similar, but in a lower risk of recurrent dislocations with surgery at the cost of surgical complications. As already stated, patients with multiple patellar dislocations are strongly advised to undergo MPFL reconstruction [6,7]. This could be the most relevant indication for ligament reconstruction, especially after the failure of conservative treatment. Usually, only elite athletes undergo MPFLR after a single dislocation.
The high patella, trochlear dysplasia, or increased TA-GT distance are predisposing factors that can certainly increase the risk of first traumatic events but at the same time their recurrence. All of the aforementioned conditions exclude the possibility of simple MPFL reconstruction due to the high risk of graft re-rupture. Therefore, associated procedures should be performed to reduce the risk of re-injury [11,12].
Surgery for objective patellofemoral instability is a tailor-made surgery by correction of the anatomical anomaly diagnosed whether bony or not [3], reconstruction of the MPFL in isolation or associated with other surgical procedures, is a technique that is not recent. It finds its place, in competition with other surgical procedures on the soft tissues, particularly in adolescents and young people in whom it is preferable not to act on the bone except in the face of significant anatomo-radiological bone defects.
Faced with one or more episodes of patella dislocation, reconstruction of the MPFL is highly recommended to provide a better functional result. In fact, multiple variations of graft sources have been suggested in the literature, including semitendinosus, gracilis, partial quadriceps, partial patellar tendons, allografts, or artificial tendons. Additionally, there are variations in patellar and femoral fixation and in the angle of knee flexion during fixation. Due to the many variables, the search for the best surgical treatment still remains to be done, even if the technique has been refined thanks to a better understanding of the origin and insertion of the ligament. The two tendons of the crow's feet (semitendinosus, gracilis) remain the most used and are very easy to remove without significant after-effects [7,11,12].
This reconstruction of the MPFL proposed and which is carried out in other centers (Lyon) resembles the Chassaing technique used since 1993 [2]. It has many strong points compared to other plastics acting only on the soft parts [4,6,13] (Goldwaith, Galeazzi, Insall, etc.) for several reasons in particular, the minimal scar damage well taken into consideration in girls, the easy adjustment of the tension of the transplant after passage through the patellar tunnel without fixation and without suture, then its recovery and fixation on the medial epicondyle in a very precise point allowing good isometry and stability of the extensor apparatus.
Fortunately, surgical procedures are more reproducible because there is consensus on the need to recreate a precise and isometric ligament through anatomical placement, including the femoral bone tunnel. The Schöttle point is the exact area where the femoral tunnel should be placed during the reconstruction procedure in order to restore the isometry of the ligament [9,10,12].
As noted, each technique has its complications. In the literature, sutures for MPFL are considered easier to perform but are not as stable as transpatellar bone tunnels (respectively 24% vs. 8.6% hypermobility). In contrast, bone tunnels carry the risk of iatrogenic fractures (0.9% - 3.6%) and the highest complication rate (21.6%) [4,12].
Overall, the cumulative complication rate after reconstruction is 26.1% according to Shah et al. which could be affected by possible poorly recorded predisposing conditions and, above all, by technical errors which represent 50% of graft failures [5,2,13].
Conclusion
Reconstruction of the MPFL is an attractive plastic surgery, it is a very interesting alternative for young girls mainly handicapped by patellofemoral instability. Often performed alone without a bone procedure in the absence of major bone abnormalities (very high TAGT index). The medium-term results are very good in our series and in the international literature.
Ideal candidates for MPFL reconstruction should be chosen after thorough evaluation and careful planning. Respecting the anchoring points, the tightening angle, and the tension of the transplant is the only guarantee of a good functional result.
Ethical consideration
The patient’s consent was obtained.
- Wang CH, Ma LF, Zhou JW, Ji G, Wang HY, Wang F, Wang J. Double-bundle anatomical versus single-bundle isometric medial patellofemoral ligament reconstruction for patellar dislocation. Int Orthop. 2013 Apr;37(4):617-24. doi: 10.1007/s00264-013-1788-6. Epub 2013 Feb 1. PMID: 23371425; PMCID: PMC3609965.
- Enderlein D, Nielsen T, Christiansen SE, Faunø P, Lind M. Clinical outcome after reconstruction of the medial patellofemoral ligament in patients with recurrent patella instability. Knee Surg Sports Traumatol Arthrosc. 2014 Oct;22(10):2458-64. doi: 10.1007/s00167-014-3164-5. Epub 2014 Jul 10. PMID: 25007722.
- Sillanpaa PJ. First-time patellar dislocation: surgery or conservative treatment. Sport Med Arthrosc. 2012; 20(3):128-135.
- Wright ML, Paul RW, Freedman KB. Medial Patellofemoral Ligament Reconstruction. Video journal of sport medicine. October 14, 2021.
- Sanchis-Alfonso V. How to Deal with Chronic Patellar Instability: What Does the Literature Tell Us? Sports Health. 2016 Jan-Feb;8(1):86-90. doi: 10.1177/1941738115604156. Epub 2015 Aug 28. PMID: 26733595; PMCID: PMC4702155.
- Aframian A, Smith TO, Tennent TD, Cobb JP, Hing CB. Origin and insertion of the medial patellofemoral ligament: a systematic review of anatomy. Knee Surg Sports Traumatol Arthrosc. 2017 Dec;25(12):3755-3772. doi: 10.1007/s00167-016-4272-1. Epub 2016 Sep 8. PMID: 27631645; PMCID: PMC5698363.
- Duthon VB. Acute traumatic patellar dislocation. Orthop Traumatol Surg Res. 2015 Feb;101(1 Suppl):S59-67. doi: 10.1016/j.otsr.2014.12.001. Epub 2015 Jan 12. PMID: 25592052.
- Fujino K, Tajima G, Yan J, Kamei Y, Maruyama M, Takeda S, Kikuchi S, Shimamura T. Morphology of the femoral insertion site of the medial patellofemoral ligament. Knee Surg Sports Traumatol Arthrosc. 2015 Apr;23(4):998-1003. doi: 10.1007/s00167-013-2797-0. Epub 2013 Dec 3. PMID: 24296991.
- Jibri Z, Jamieson P, Rakhra KS, Sampaio ML, Dervin G. Patellar maltracking: an update on the diagnosis and treatment strategies. Insights Imaging. 2019 Jun 14;10(1):65. doi: 10.1186/s13244-019-0755-1. PMID: 31201575; PMCID: PMC6570735.
- Fujino K, Tajima G, Yan J, Kamei Y, Maruyama M, Takeda S, Kikuchi S, Shimamura T. Morphology of the femoral insertion site of the medial patellofemoral ligament. Knee Surg Sports Traumatol Arthrosc. 2015 Apr;23(4):998-1003. doi: 10.1007/s00167-013-2797-0. Epub 2013 Dec 3. PMID: 24296991.
- Mayer P, Schuster P, Schlumberger M, Eichinger M, Pfaff M, Immendörfer M, Richter J. Midterm Results after Implant-Free Patellar Fixation Technique for Medial Patellofemoral Ligament Reconstruction. J Knee Surg. 2020 Nov;33(11):1140-1146. doi: 10.1055/s-0039-1692654. Epub 2019 Jul 3. PMID: 31269526.
- Tao F, Tao H, Jin L, Gao H, Luo Y, Zhang Z. Isolated medial patellofemoral ligament reconstruction improves static bipedal balance control in young patients with recurrent lateral patellar instability. J Orthop Surg Res. 2023 Oct 12;18(1):771. doi: 10.1186/s13018-023-04272-9. PMID: 37828531; PMCID: PMC10571255.
- Kay J, Memon M, Ayeni OR, Peterson D. Medial Patellofemoral Ligament Reconstruction Techniques and Outcomes: A Scoping Review. Curr Rev Musculoskelet Med. 2021 Dec;14(6):321-327. doi: 10.1007/s12178-021-09719-2. Epub 2021 Dec 11. PMID: 34893964; PMCID: PMC8733066.
Article Alerts
Subscribe to our articles alerts and stay tuned.
 This work is licensed under a Creative Commons Attribution 4.0 International License.
This work is licensed under a Creative Commons Attribution 4.0 International License.








 Save to Mendeley
Save to Mendeley
