Journal of Clinical Research and Ophthalmology
Multimodal Imaging in Gyrate Atrophy: Diagnostic Insights from Fundus Photography and Autofluorescence
Vaishali Tomar*, Padma Chorol, Swarna Nishu, Shihana J Parveen and Aakanksha Raghuvanshi
Guru Nanak Eye Centre, Maulana Azad Medical College, Delhi, India
Cite this as
Tomar V, Chorol P, Nishu S, Parveen SJ, Raghuvanshi A. Multimodal Imaging in Gyrate Atrophy: Diagnostic Insights from Fundus Photography and Autofluorescence. J Clin Res Ophthalmol. 2025;12(2):009-010. Available from: 10.17352/2455-1414.000109Copyright License
© 2025 Tomar V, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.A 22-year-old male presented with progressively worsening night vision and peripheral visual field constriction over the past few years. Notably, he reported that his younger sister exhibited similar symptoms, suggesting a hereditary pattern. Best-corrected visual acuity was markedly reduced to finger counting at two meters in both eyes. Intraocular pressures were within normal limits—9 mmHg in the right eye and 11 mmHg in the left eye. Anterior segment examination revealed no abnormalities.
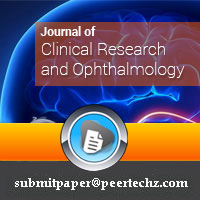
Fundus examination of both eyes showed well-defined optic discs with surrounding peripapillary atrophy. The foveal reflex was dull, and the retina was attached. Strikingly, there was symmetric, well-demarcated chorioretinal atrophy involving the mid-periphery, with centripetal extension toward the posterior pole (Figure 1). The maculae were relatively spared, though with subtle changes. Optical coherence tomography (OCT) revealed a distorted foveal contour and the presence of epiretinal membranes in both eyes. While there was no gross retinal traction, subtle wrinkling of the inner retinal surface suggested minimal retinal distortion. The outer retinal layers appeared thinned, consistent with photoreceptor degeneration.
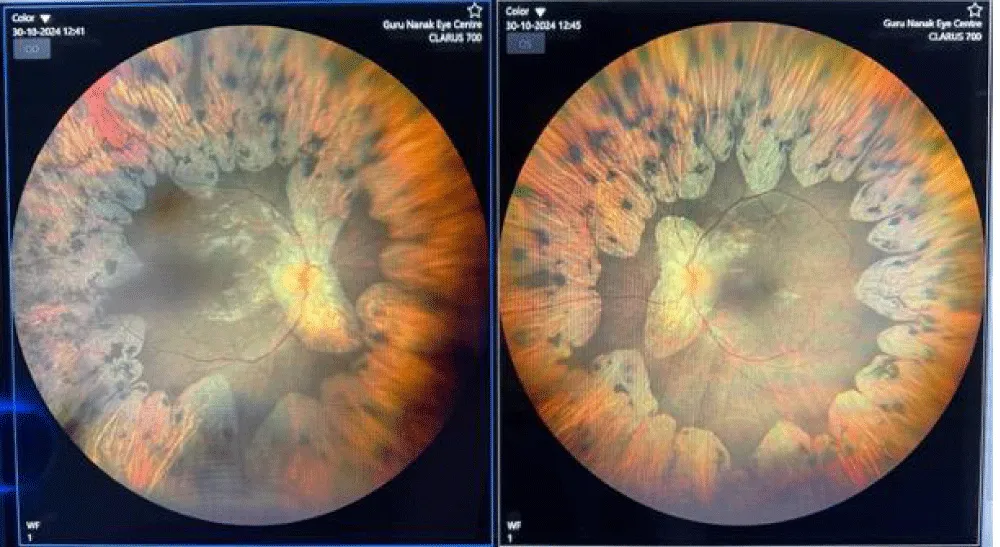
Fundus autofluorescence imaging demonstrated sharply demarcated zones of hypoautofluorescence in the mid-periphery and posterior pole. These areas closely corresponded to the visible chorioretinal atrophy and in some regions extended slightly beyond, sparing the central macula, producing a classic “scalloped” pattern of atrophy (Figure 2). The autofluorescence findings were symmetrical between the two eyes.
Transitioning from clinical observations to disease mechanisms, the constellation of clinical findings, family history, and imaging features led to a diagnosis of gyrate atrophy of the choroid and retina. This was confirmed biochemically by elevated plasma ornithine levels. Gyrate atrophy is a rare autosomal recessive chorioretinal dystrophy caused by mutations in the OAT gene (ornithine aminotransferase), leading to ornithine accumulation and subsequent retinal toxicity [1]. Patients typically present in the first two decades of life with nyctalopia, progressive peripheral vision loss, and eventual central vision impairment. Characteristic fundus findings include sharply demarcated scalloped areas of chorioretinal atrophy that begin in the mid-periphery and advance centripetally [2].
Early diagnosis is essential, as treatment strategies such as dietary arginine restriction and vitamin B6 (pyridoxine) supplementation may help reduce plasma ornithine levels and slow disease progression in responsive individuals [3]. OAT mutations exhibit variability in their expression, and some genotypes may be more responsive to pyridoxine supplementation than others. Genetic testing is thus instrumental in identifying pyridoxine-responsive mutations and can guide management. Additionally, screening of family members is critical given the autosomal recessive inheritance. Zonular weakness and lens instability may also be associated with this condition, posing challenges during cataract surgery [4].
This case underscores the importance of multimodal imaging—especially fundus autofluorescence and OCT—in the early recognition and characterization of gyrate atrophy. Even in advanced stages with poor vision, these imaging modalities provide valuable insight into disease pattern and macular involvement. Additionally, systemic metabolic screening based on ocular signs can guide timely diagnosis and potential therapeutic interventions.
Gyrate atrophy should be considered in young patients presenting with night blindness, peripheral visual field loss, and characteristic scalloped areas of chorioretinal degeneration. Integration of multimodal imaging with biochemical and genetic evaluation offers a comprehensive approach to diagnosis and monitoring.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. The patients understand that names and initials will not be published, and efforts will be made to conceal their identity.
- Balfoort BM, Buijs MJN, ten Asbroek ALMA, Bergen AAB, Boon CJF, Ferreira EA, et al. A review of treatment modalities in gyrate atrophy of the choroid and retina (GACR). Mol Genet Metab. 2021;134(1-2):27–36. Available from: https://doi.org/10.1016/j.ymgme.2021.07.010
- Potter MJ, Berson EL. Diagnosis and treatment of gyrate atrophy. Int Ophthalmol Clin. 1993;33(2):121–36. Available from: https://pubmed.ncbi.nlm.nih.gov/8325736/
- Ohkubo Y, Ueta A, Ito T, Sumi S, Yamada M, Ozawa K, et al. Vitamin B6-responsive ornithine aminotransferase deficiency with a novel mutation G237D. Tohoku J Exp Med. 2005;205(4):335–40. Available from: https://doi.org/10.1620/tjem.205.335
- Chao JT, Rao P, Hart JC. Zonular weakness in patients with gyrate atrophy of the choroid and retina. JCRS Online Case Rep. 2017;5(4):17–9. Available from: https://journals.lww.com/jcro/fulltext/2017/10000/zonular_weakness_in_patients_with_gyrate_atrophy.5.
Article Alerts
Subscribe to our articles alerts and stay tuned.
 This work is licensed under a Creative Commons Attribution 4.0 International License.
This work is licensed under a Creative Commons Attribution 4.0 International License.

 Save to Mendeley
Save to Mendeley
