Journal of Clinical Research and Ophthalmology
Acute vision threatening thyroid orbitopathy associated with cataract surgery: A case series and review of the literature
Christopher R Dermarkarian1, Seanna R Grob2 and Kenneth A Feldman3
2Orbit and Oculofacial Plastic and Reconstructive Surgery, Department of Ophthalmology, University of California, San Francisco, CA, USA
3Orbit and Oculofacial Plastic and Reconstructive Surgery, Kaiser Permanente South Bay, Los Angeles, CA, USA
Cite this as
Dermarkarian CR, Grob SR, Feldman KA (2024) Acute vision threatening thyroid orbitopathy associated with cataract surgery: A case series and review of the literature. J Clin Res Ophthalmol 11(1): 011-016. DOI: 10.17352/2455-1414.000105Copyright License
© 2024 Dermarkarian CR, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.Thyroid eye disease can be associated via cataract surgery with devastating visual consequences. A systematic review of the clinical records of patients with aggravation of their thyroid orbitopathy after eye surgery at a tertiary facility was performed. Patients who had worsening of their thyroid orbitopathy within the post-operative period of cataract surgery were included. Clinical findings were reviewed including clinical examination and imaging. A literature review was also performed. Two patients who underwent cataract surgery and presented with newly diagnosed and severe thyroid orbitopathy post-operatively were identified. Both patients were male, averaging 71 years of age. Both patients noticed symptoms of diplopia within one week after cataract surgery and had clinical and imaging findings consistent with severe thyroid orbitopathy. Both patients required urgent bilateral orbital decompression due to compressive optic neuropathy. Visual acuity was preserved in both patients. The average follow-up was 6 years. Males who have activation of TED after cataract surgery appear to have a higher risk of developing compressive optic neuropathy and require immediate intervention, which is consistent with male gender as a risk factor for severe disease. Patients with thyroid disease should be counselled pre-operatively about the risk of disease aggravation after cataract surgery.
Introduction
Cataract surgery is one of the most commonly performed surgical procedures. Due to the fast-growing segment of the population that is over 65 years of age, the volume of cataract surgery is on the rise, creating an increasing workload for ophthalmologists [1-4]. A thorough preoperative evaluation of the patient is necessary, which historically included evaluation of the need for cataract surgery and informed consent. However, along with an increase in population size, patient expectations, phacoemulsification techniques, and technology have continued to evolve. Consequently, the pre-operative visit has expanded to also include extensive discussions about surgical, lens, refractive, and laser options, all of which have financial and medical considerations. Given the time constraints placed on physicians for length of appointment time, it can be challenging to cover all of this information in addition to performing a thorough medical history and examination.
There are a number of systemic and ocular diseases that can affect the outcome of cataract surgery. A history of thyroid disease or Thyroid Eye Disease (TED) or clinical examination findings concerning either are additional factors to explore prior to surgical intervention. TED is an autoimmune inflammatory disorder that occurs in 25% - 75% of dysthyroid patients, which can include hyperthyroidism, hypothyroidism, and euthyroidism [5,6]. The incidence of TED is 2.9 per 100,000 males and 16 per 100,000 females [7]. Risk factors for developing TED include smoking, life stressors, poorly controlled hypothyroidism following radioactive iodine, and family history [8-10]. Predictive factors for developing more serious sequela from TED include increasing age, male gender, smoking, radioactive iodine therapy, diabetes, and rapid onset of disease [11].
Previous literature has reported the aggravation of TED by periocular injections (botulinum toxin), medications (corticosteroid and rosiglitazone), ocular surgery (cataract surgery, strabismus surgery, and orbital decompression), and retrobulbar anesthesia injections [12-22]. TED activation has also been described in patients without a known history of TED, following cataract surgery, laser in-situ keratomilieusis, facelift in combination with blepharoplasty, laser resurfacing, forehead lift, filler injections, and botulinum toxin injections [17,21,23]. We present a series of patients who did not have a known history of TED who presented post-operatively after cataract surgery with severe and aggressive TED that required numerous visits for management and preservation of sight. In addition, a literature review of all cases of thyroid eye disease activation after cataract surgery was performed.
Methods
This case series was conducted in compliance with the rules and regulations of the Health Insurance Portability and Accountability Act and all applicable federal and state laws and in adherence to the tenets of the Declaration of Helsinki. Patient consent for publication was not obtained as there are no readily identifiable patient identifiers found within this manuscript.
Patients presenting to a tertiary care facility with acute worsening of thyroid orbitopathy after eye surgery were reviewed between 2011 and 2018. Electronic medical records for these patients were collated and information regarding age at presentation, gender, symptoms and signs, disease onset, timing of disease onset after surgery, imaging findings, management, and clinical outcome was extracted. All imaging studies were reviewed. Results are presented in descriptive format.
A literature search in the PubMed database was performed using the following terms and
Boolean operators: (“Thyroid”) AND (“Reactivation” OR “Active” OR “Acute”) AND (“Cataract Surgery”). Inclusion criteria included published articles indexed within the PubMed database, reports published in the English language, and cases describing thyroid eye disease activation after cataract surgery. Cases were abstracted for clinical characteristics.
Case reports
Patient #1
A 74-year-old male with a past ocular history of a branch retinal vein occlusion on the left with intravitreal anti-Vascular Endothelial Growth Factor (VEGF) treatments and narrow angles status post bilateral laser peripheral iridotomy underwent cataract surgery on the left eye. His preoperative visual acuity was 20/100 on the right and 20/80 on the left. Exactly one week after uneventful cataract surgery, the patient had a decrease in vision to 20/150 bilaterally and a decline in color vision bilaterally with congested orbits and restriction of extraocular muscles.
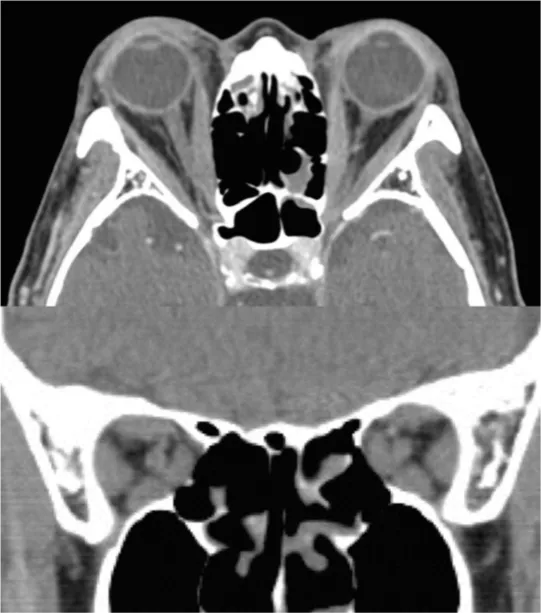
Thyroid stimulating hormone was low at 0.1 mIU/L. Free T4 was within normal limits. CT and MRI imaging revealed significantly enlarged rectus muscles bilaterally with compression of the nerve at the apex concerning compressive optic neuropathy from thyroid eye disease (Figure 1). The patient was given urgent intravenous methylprednisolone (1 gram daily for 3 consecutive days) with mild improvement in vision initially but then experienced a quick decline in vision to count fingers with frozen globes and significant proptosis resulting in corneal decompensation bilaterally. The patient was taken for urgent bilateral endoscopic orbital decompression of the floor and medial walls. He required nasal tarsorrhaphies bilaterally post-operatively for treatment of corneal breakdown. He received additional doses of intravenous steroids and then was continued on oral steroids by his general ophthalmologist. Approximately two weeks after decompression surgery, the patient’s vision had improved to 20/400 bilaterally and the edema and chemosis continued to improve over the following few weeks. He was then referred for orbital radiation (2000 cGY over 10 days). At 3 months post-operatively, the patient had visual acuities of 20/50 on the right and 20/60 on the left. Final visual acuity was 20/25 on the right and 20/40 on the left 6 years later with full-color vision bilaterally. At the last follow-up visit, there was a positive afferent pupillary defect on the right and a constricted visual field. The patient also had an esotropia that was managed well with prisms. The patient had a total of 142 encounters since the initial presentation of acute thyroid orbitopathy after cataract surgery.
Patient #2
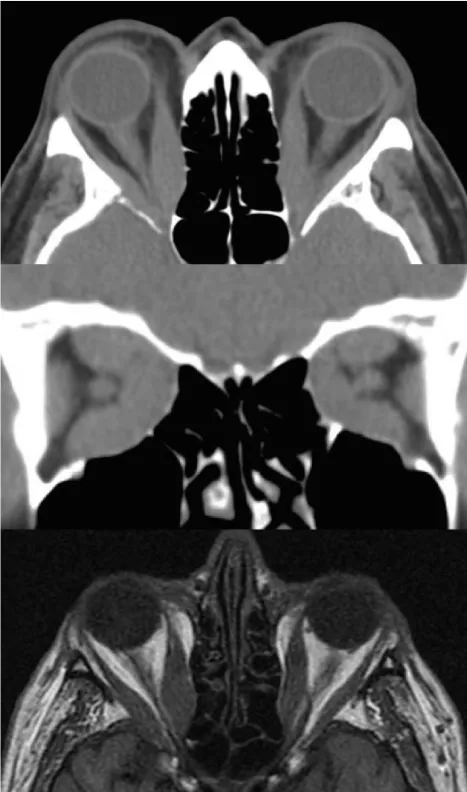
A 69-year-old male with no past ocular history and a past medical history of diabetes mellitus and Graves hyperthyroidism status post radioactive iodine treatment and a 63-pack-year smoking history presented for a cataract evaluation. He was found to have visual acuities of 20/100 on the right and 20/80 on the left with nuclear sclerosis bilaterally. The patient underwent uneventful bilateral cataract surgery done 2 months apart. Post-operative day 1 after cataract surgery on the right (second) eye there was a question of a possible decompensating esotropia. Seventeen days after the second cataract surgery, the patient presented with a significant decline in his vision on the right to 20/300. He had an afferent pupillary defect and a loss of color vision. Examination showed proptosis and significant limitation in extraocular motility in all directions. Thyroid labs were abnormal (thyroid stimulating hormone 0.25 mIU/L, thyroid peroxidase Ab 74.4 IU/ml, Thyroid stimulating immunoglobulin 491 percent of baseline). Imaging showed significant enlargement of all rectus muscles bilaterally with nerve compression at the apex that was worse on the right (Figure 2). The patient was given urgent intravenous methylprednisolone (1 gram daily for 3 consecutive days) with improvement in his vision to 20/70 on the right. He was referred for urgent orbital radiation therapy (2000cGy over 10 days) bilaterally. After treatment, his vision was 20/100 on the right and 20/30 on the left with improvement in his visual field testing on the right, but there was a persistent afferent pupillary defect, low color vision, and a temporal visual field depression on the right. Subsequently, the patient continued to decline to count fingers vision on the right. The patient was again started on oral steroids and scheduled for an urgent right endoscopic decompression of the floor and medial wall. Post-operatively his vision remained count fingers on the right so additional intravenous methylprednisolone was given (1 gram daily for 3 consecutive days). He was then taken back to the operating room for a right lateral wall decompression of bone and removal of intraconal fat roughly one week later and then was slowly tapered off the oral steroids.
The final documented visual acuity 4 years after decompression surgery was 20/60 on the right and 20/20 on the left. The patient did have a large esotropia (95 prism diopters) after decompression surgery requiring a large bilateral medial rectus recession. The patient had a total of 65 encounters since the initial presentation of acute thyroid orbitopathy after cataract surgery.
Discussion
Thyroid eye disease is a disease entity that should be considered pre- and post-operatively for cataract surgery. When the classic orbital and eyelid findings are seen, the diagnosis of thyroid eye disease is usually fairly straightforward. However, when physicians encounter patients without a history of thyroid disease or with subtle or no ophthalmologic findings, disease diagnosis may be missed or present a challenge to detect pre-operatively. Also, the absence of double vision prior to cataract surgery in thyroid patients may be the result of poor vision from the cataract, precluding the ability to detect this prior to the restoration of sight [15]. Therefore, surgeons should maintain a high level of suspicion if subtle findings are seen on the exam and refer the patient for laboratory workup for thyroid disease.
Previous studies have suggested that local trauma and increased orbital pressure may play a role in thyroid eye disease [24,25]. The etiology of TED is thought to be due to the activation of orbital fibroblasts by T and B lymphocytes and other inflammatory cells from the production of cytokines. Release of these chemical transmitters during cataract surgery could trigger the TED inflammatory cascade leading to activation or aggravation of disease [21,23,26]. During surgery, manipulation of the periocular tissues or the globe, use of anesthetic agents that are known to be myotoxic, surgical stress, and post-operative inflammation can all contribute to increasing the risk of precipitating TED in susceptible patients [21,24,25,27].
Our two patients had newly diagnosed, acute onset, rapidly progressing, and aggressive thyroid eye disease after cataract surgery. Both patients presented with symptoms within a week of their last cataract surgery and had bilateral orbital findings on examination and imaging. Both patients had sight-threatening optic neuropathy – one bilaterally, and one on the right. Both patients required urgent intravenous steroids and both underwent orbital decompression and orbital radiation therapy. Both patients required numerous clinical visits after cataract surgery.
Both of our patients had risk factors for severe TED. Both patients were males and older in age. Patient #2 also had diabetes, a history of radioactive iodine therapy, and a 65-pack-year smoking history. Only Patient #2 had a history of known thyroid disease; Patient #1 had no known history of thyroid disease or other autoimmune diseases. Neither patient had a history of orbital thyroid disease.
The percentage of patients with TED who undergo cataract surgery remains low [28]. Reactivation of TED after cataract surgery is a rare phenomenon. A summary of the current literature regarding TED activity after cataract surgery can be seen in Table 1. Yi, et al. presented five cases of patients who developed TED after cataract surgery [17]. Two were male and three were female with a mean age of 54.6 years. All patients in this series had a known history of thyroid disease prior to cataract surgery. All had received systemic thyroid treatment via oral treatment and radioactive iodine therapy. Three of the patients had signs of TED preoperatively, and two did not. At presentation, 3 were euthyroid and 2 were hyperthyroid. Two were diabetic and one had a 60-year smoking history. All presented with symptoms within a mean of 7.4 weeks after cataract surgery. Two of the patients in this series had severe disease with optic neuropathy like our cases. Both of them were elderly males with diabetes. One of these patients had complete loss of vision due to no light perception.
Kim, et al. presented two cases of patients with thyroid orbitopathy after cataract surgery – one with a known history of thyroid disease and one without [23]. Both were female with an average age of 74.5 years. One presented 4 weeks after surgery and the other 6 weeks. Both presented with lid retraction, diplopia, and proptosis and one had compressive optic neuropathy.
Interestingly, both patients had retrobulbar anesthesia for their cataract surgery.
Wai, et al. presented a case of a 66-year-old Chinese male with a known history of TED who had cataract surgery in the right eye followed by the left eye 12 years later [21]. Both surgeries utilized retrobulbar anesthesia. Three weeks after the second eye surgery, the patient presented with diplopia with severe restriction of extraocular motility. Due to progressive proptosis, he developed exposure keratopathy requiring 3-wall orbital decompression. Even after decompression, the patient developed compressive optic neuropathy when steroid taper was attempted and subsequently was treated with orbital radiotherapy due to complications from chronic steroid use.
Shadpour, et al. also presented a case of an 80-year-old woman who had a known history of TED that was quiescent for 4 years prior to cataract extraction [16]. She had rapidly progressive TED bilaterally after cataract surgery of the right eye which lasted for 1 year. After 2 years of stability, she had cataract surgery on the left eye, and again TED worsened bilaterally. She received retrobulbar anesthesia for the right eye and peribulbar for the left. She presented within one month of surgery with thyroid eye symptoms including diplopia and restriction of extraocular motility, eyelid retraction, and periorbital edema. Her sequential and bilateral symptoms after each cataract surgery show that with each surgery, inflammation was activated causing progressive disease.
It is difficult to draw any specific conclusions regarding TED activation after cataract surgery given the small sample size in our review. However, some interesting observations can be drawn with the addition of our two case reports. The average age of those with TED activation after cataract surgery is 65.7 years of age; this is younger than compared to the average age of patients undergoing cataract surgery (73.8 years) [29]. TED activation after cataract surgery appears to affect both males (47%) and females (53%) equally. Males who have activation of TED after cataract surgery appear to have a higher risk of developing compressive optic neuropathy and require immediate intervention, which is consistent with male gender as a risk factor for severe disease. Though the data is limited, the average time to symptom presentation after cataract surgery is 5.29 weeks. Though not seen in our case series, those who received retrobulbar anesthesia (67%) were more likely to have activation of TED after cataract surgery compared to those who did not (33%). Most importantly, the risk of compressive optic neuropathy remains high (36%) in this disease entity. Of note, the patients seen in both the case series and literature review were treated prior to the mainstream use of tocilizumab and teprotumumab for thyroid eye disease. It is unclear how the use of these medications may have prevented the complications and vision loss seen in this patient population.
For patients with a known history of thyroid disease or thyroid eye disease, surgeons should inform patients of the risks of thyroid eye disease activation or aggravation and patients should be watched carefully post-operatively for any signs of orbital disease. Surgeons should maintain a high level of suspicion for TED if they present for cataract surgery with any associated findings, such as injection, proptosis, chemosis, limitation of extraocular motility, retraction, or eyelid swelling. Additional study is needed to determine the risk factors associated with TED activation after cataract surgery.
- Hatch WV, Campbell Ede L, Bell CM, El-Defrawy SR, Campbell RJ. Projecting the growth of cataract surgery during the next 25 years. Arch Ophthalmol. 2012 Nov;130(11):1479-81. doi: 10.1001/archophthalmol.2012.838. PMID: 23143457.
- Etzioni DA, Liu JH, Maggard MA, Ko CY. The aging population and its impact on the surgery workforce. Ann Surg. 2003 Aug;238(2):170-7. doi: 10.1097/01.SLA.0000081085.98792.3d. PMID: 12894008; PMCID: PMC1422682.
- Erie JC. Rising cataract surgery rates: demand and supply. Ophthalmology. 2014 Jan;121(1):2-4. doi: 10.1016/j.ophtha.2013.10.002. PMID: 24388393.
- Gollogly HE, Hodge DO, St Sauver JL, Erie JC. Increasing incidence of cataract surgery: population-based study. J Cataract Refract Surg. 2013 Sep;39(9):1383-9. doi: 10.1016/j.jcrs.2013.03.027. Epub 2013 Jun 29. PMID: 23820302; PMCID: PMC4539250.
- Glaser JS. Graves' ophthalmopathy. Arch Ophthalmol. 1984; 102(10): 1448-9.
- Sergott RC, Glaser JS. Graves' ophthalmopathy. A clinical and immunologic review. Surv Ophthalmol. 1981 Jul-Aug;26(1):1-21. doi: 10.1016/0039-6257(81)90120-x. PMID: 6895125.
- McAlinden C. An overview of thyroid eye disease. Eye Vis (Lond). 2014 Dec 10;1:9. doi: 10.1186/s40662-014-0009-8. PMID: 26605355; PMCID: PMC4655452.
- Bartley GB. The epidemiologic characteristics and clinical course of ophthalmopathy associated with autoimmune thyroid disease in Olmsted County, Minnesota. Trans Am Ophthalmol Soc. 1994;92:477-588. PMID: 7886878; PMCID: PMC1298522.
- Kendall-Taylor P, Perros P. Clinical presentation of thyroid associated orbitopathy. Thyroid. 1998 May;8(5):427-8. doi: 10.1089/thy.1998.8.427. PMID: 9623736.
- Rootman J, Dolman P. Thyroid orbitopathy. In: Diseases of the orbit: a multidisciplinary approach. Philadelphia: Lippincott Williams & Wilkins. 2003; 169–212.
- Dolman PJ, Rootman J. Predictors of disease severity in thyroid-related orbitopathy. (Chap 18) Orbital disease. Present status and future challenges. Boca Raton: Taylor and Francis. 2005.
- Korn BS, Seo SW, Levi L, Granet DB, Kikkawa DO. Optic neuropathy associated with botulinum A toxin in thyroid-related orbitopathy. Ophthalmic Plast Reconstr Surg. 2007 Mar-Apr;23(2):109-14. doi: 10.1097/IOP.0b013e318032eb12. PMID: 17413623.
- Gupta OP, Boynton JR, Sabini P, Markowitch W Jr, Quatela VC. Proptosis after retrobulbar corticosteroid injections. Ophthalmology. 2003 Feb;110(2):443-7. doi: 10.1016/S0161-6420(02)01743-8. PMID: 12578795.
- Levin F, Kazim M, Smith TJ, Marcovici E. Rosiglitazone-induced proptosis. Arch Ophthalmol. 2005 Jan;123(1):119-21. doi: 10.1001/archopht.123.1.119. PMID: 15642828.
- Hamed LM, Lingua RW. Thyroid eye disease presenting after cataract surgery. J Pediatr Ophthalmol Strabismus. 1990 Jan-Feb;27(1):10-5. doi: 10.3928/0191-3913-19900101-04. PMID: 2182823.
- Shadpour JM, Menghani RM, Douglas RS, Goldberg RA, Tsirbas A. Reactivation of thyroid-associated orbitopathy after cataract surgery. Jpn J Ophthalmol. 2009 Jan;53(1):44-46. doi: 10.1007/s10384-008-0607-x. Epub 2009 Jan 30. PMID: 19184309.
- Yi BP, Leng SL, Kwang LB, Rootman J. Development of thyroid-related orbitopathy following cataract surgery. Orbit. 2009;28(6):383-7. doi: 10.3109/01676830903071232. PMID: 19929665.
- Xu L, Glass LR, Kazim M. Reactivation of thyroid eye disease following extraocular muscle surgery. Ophthalmic Plast Reconstr Surg. 2014 Jan-Feb;30(1):e5-6. doi: 10.1097/IOP.0b013e3182873cfe. PMID: 23467286.
- Campbell A, Whittaker TJ, Sokol JA. Re: "Reactivation of thyroid eye disease following extraocular muscle surgery". Ophthalmic Plast Reconstr Surg. 2014;30(4):353.
- Baldeschi L, Lupetti A, Vu P, Wakelkamp IM, Prummel MF, Wiersinga WM. Reactivation of Graves' orbitopathy after rehabilitative orbital decompression. Ophthalmology. 2007 Jul;114(7):1395-402. doi: 10.1016/j.ophtha.2006.10.036. Epub 2007 Feb 22. PMID: 17320178.
- Wai DC, Ho SC, Seah LL, Fong KS, Khoo DH. Severe Graves' ophthalmopathy after retrobulbar anesthesia for cataract extraction in a patient with mild stable thyroid eye disease. Thyroid. 2003 Aug;13(8):823-6. doi: 10.1089/105072503768499725. PMID: 14558926.
- Han SK, Hwang JM. Thyroid disease and vertical rectus muscle overaction after retrobulbar anesthesia. J Cataract Refract Surg. 2003 Jan;29(1):78-84. doi: 10.1016/s0886-3350(02)01437-2. PMID: 12551671.
- Kim SJ, Kim BJ, Lee HB, Tsirbas A, Kazim M. Thyroid associated orbitopathy following periocular surgery. Korean J Ophthalmol. 2006 Jun;20(2):82-6. doi: 10.3341/kjo.2006.20.2.82. PMID: 16892642; PMCID: PMC2908832.
- Feldon SE, Muramatsu S, Weiner JM. Clinical classification of Graves' ophthalmopathy. Identification of risk factors for optic neuropathy. Arch Ophthalmol. 1984 Oct;102(10):1469-72. doi: 10.1001/archopht.1984.01040031189015. PMID: 6548373.
- Rapoport B, Alsabeh R, Aftergood D, McLachlan SM. Elephantiasic pretibial myxedema: insight into and a hypothesis regarding the pathogenesis of the extrathyroidal manifestations of Graves' disease. Thyroid. 2000 Aug;10(8):685-92. doi: 10.1089/10507250050137761. PMID: 11014313.
- Kazim M, Goldberg RA, Smith TJ. Insights into the pathogenesis of thyroid-associated orbitopathy: evolving rationale for therapy. Arch Ophthalmol. 2002 Mar;120(3):380-6. doi: 10.1001/archopht.120.3.380. PMID: 11879144.
- Rainin EA, Carlson BM. Postoperative diplopia and ptosis. A clinical hypothesis based on the myotoxicity of local anesthetics. Arch Ophthalmol. 1985 Sep;103(9):1337-9. doi: 10.1001/archopht.1985.01050090089038. PMID: 4038126.
- Strong Caldwell A, Patnaik JL, Ackerman M, Christopher KL, Lynch AM, Singh JK. Risk of Refractive Prediction Error After Cataract Surgery in Patients with Thyroid Eye Disease. Clin Ophthalmol. 2021 Nov 11;15:4431-4438. doi: 10.2147/OPTH.S337360. PMID: 34795474; PMCID: PMC8593354.
- Terveen D, Berdahl J, Dhariwal M, Meng Q. Real-World Cataract Surgery Complications and Secondary Interventions Incidence Rates: An Analysis of US Medicare Claims Database. J Ophthalmol. 2022 Apr 6;2022:8653476. doi: 10.1155/2022/8653476. PMID: 35433042; PMCID: PMC9007656.
Article Alerts
Subscribe to our articles alerts and stay tuned.
 This work is licensed under a Creative Commons Attribution 4.0 International License.
This work is licensed under a Creative Commons Attribution 4.0 International License.

 Save to Mendeley
Save to Mendeley
