Imaging Journal of Clinical and Medical Sciences
Critical intracranial hypertension of hidden etiology
Gamiz-Gamiz A1*, Abril-Molina A1, Gomez-Luque JM1, Saura Rojas E2, Pastor-Rull J3 and Ocete-Hita E1
2Neurosurgery, University Hospital Complex of Granada, Spain
3Neurorradiology, University Hospital Complex of Granada, Spain
Cite this as
Gamiz-Gamiz A, Abril-Molina A, Gomez-Luque JM, Saura Rojas E, Pastor-Rull J, et al. (2019) Critical intracranial hypertension of hidden etiology. Imaging J Clin Medical Sci 6(1): 087-088. DOI: 10.17352/2455-8702.000126Introduction
Arachnoid cysts are central nervous system lesions that infrequently occur in childhood. They can be mobile and produce partial or complete obstruction in the Cerebrospinal Fluid (CSF) circulation. They are usually present at birth and are asymptomatic, although sometimes the symptoms appear in adolescence or adulthood due to the growth acceleration [1,2].
Depending on their size and location, they may produce neurological symptoms due to a blockage of the CSF flow through the ventricular system such as intermittent headache, drops attack or the "Booble-head doll syndrome"; which consists of continuous head movements forwards and backwards with a frequency of 2Hz-3Hz. Fortunately, even intracranial hypertension symptoms are the most severe, they are not common.
Radiological diagnosis can be difficult and it is based on the clinical suspect due to the fact that very specific imaging techniques are needed [1,3].
Clinical Report
We present the case of a 7-year-old male patient, admitted to the pediatric intensive care unit with critical intracranial hypertension demonstrated by Computed Tomography (CT).
Several hours before admission the patient started with intense oppressive holocraneal headache associated with vomiting, progressive drowsiness, incoherent language and poor response to stimulation.
Exploration
Glasgow 8/15. Heart rate 70 beats/minute, respiratory rate 11 breaths/minute, blood pressure 110mmHg /57mmHg, 96% oxygen saturation without oxygen therapy. Arreactive isocoric middle pupils, normal osteotendinous reflexes, absence of meningeal signs Rest of the exploration without other pathological findings.
Complementary tests
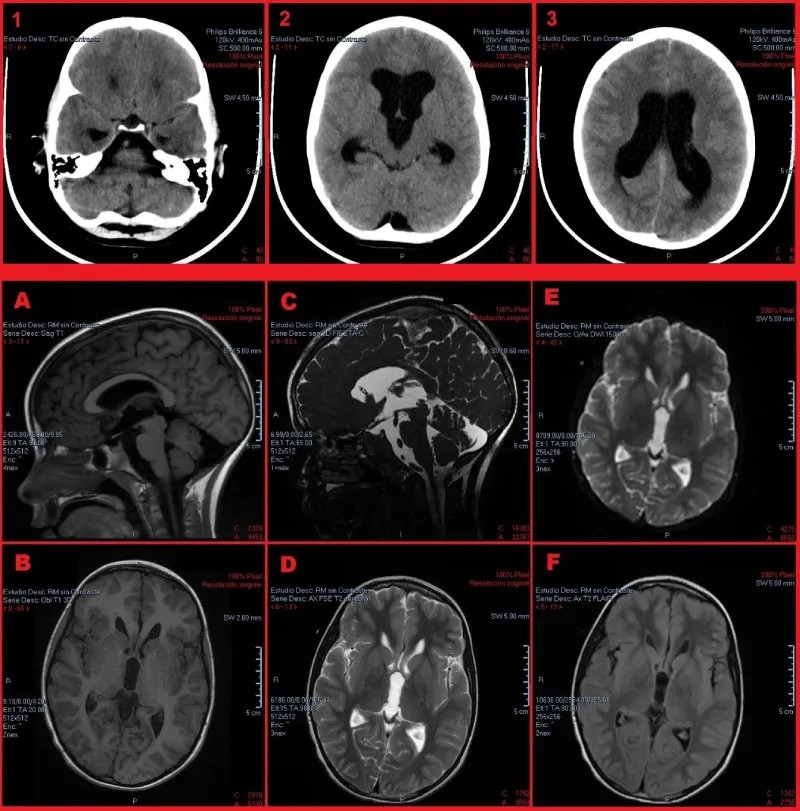
The cranial CT showed dilatation of lateral ventricles and the third ventricle with signs of critical intracranial hypertension but there were no evidences of space-occupying lesions that product obstructive hydrocephalus. (image 1.1, 1.2, 1.3). Blood cell account, biochemistry and coagulation test were made and no disturbances were found.
Evolution
Endotracheal intubation was performed, dexamethasone was administered and urgently transferred to the operating room to set an external ventricular drainage (DVE). The patient had a progressive improvement in his neurological state. Once the patient was stabilized, a scheduled Magnetic Resonance Imaging (MRI) was performed in which normalization of the ventricular size was observed and the existence of a thin septum in the anterior region of the III ventricle was described. The septum did not occlude the forages of Monro and Silvio and therefore did not justify the development of hypertensive hydrocephalus (Image 1).
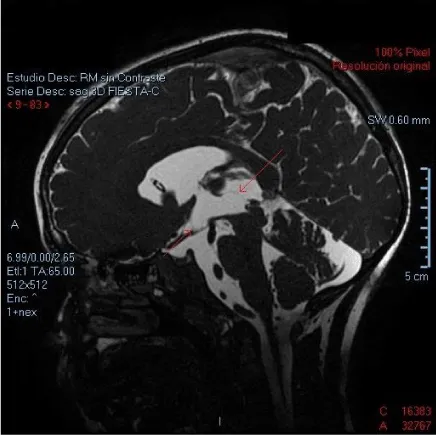
A high resolution MRI was requested to define the characteristics of this septum. Specifically, the Fast Imaging Employing Steady-state Acquisition (FIESTA) sequence was taken. This is a specific sequence that could demonstrated a slim linear image in the anterior region of the III ventricle that subsequently imprinted in the gray intertermal commissure. A linear image was identified that apparently excludes the optic and infundibular recesses of the III ventricle, with slight anterior protrusion of the terminalis lamina (Image 2). Finally with the complete outline, the arachnoid cysts diagnosis was made.
Endoscopic ventriculostomy for cyst exeresis was made without any surgical complication. Currently, the patient is asymptomatic and a post-surgical cranial MRI was performed that demonstrated a permeable ventricular system.
Discussion
Obstructive hydrocephalus are often caused by space-occupying lesions, but sometimes these can be difficult to discover if the correct MRI sequence is untaken.
There is a wide variety of ventricular cystic lesions whose differential diagnosis is usually made by a radiological study, although the final confirmation must be made by histopathological studies. These include: arachnoid cyst, colloid cyst, epidermal and dermoid cyst, endodermal, neuroepithelial, "Rathke's cleft cyst", and other entities such as neurocysticercosis or cerebral hydatidosis [1,3]. Arachnoid cysts are collections of CSF bounded by a membrane of arachnoid tissue that may or may not communicate with the subarachnoid space.
They represent 1% of space-occupying lesions although it is an under diagnosed pathology since they can be asymptomatic or have difficult radiological diagnosis. Its origin is unknown, some appearing congenitally and others secondary to adhesion after various traumatic-inflammatory processes. It is believed that the liquid inside can increase its size by diffusion or by valvulated mechanism.
They are usually located on the brain surface, more frequently in the fissures although they can also be founded inside the ventricles. Therefore the clinical manifestation might be completely different depending on the location of the cyst. While the patient described here debuted with acute intracranial hypertension, other patients could manifest focal neurological symptoms if the arachnoid cysts were placed at the cerebral cortex. These lesions occur isolated or associated with other malformations such as of the corpus callosum agenesia, cerebellar lobulation deficit, absence of septum pellucidum or metabolic diseases such as glutaric aciduria type I [1,3].
MRI is the goal standard diagnostic test. Arachnoid cysts can be identified as well delimited lesions with a slim isointense layer and content of the same characteristics as the CSF (hypointense T1 sequence and hyperintense in T2 sequence that does not capture gadolinium). But as in the presented case, conventional RMI isn´t not always enough to find them, and in these cases and when the clinical diagnostic suspicion is high; it is indicated to make special sequences of very fine cuts such as the FIESTA sequence. The equivalent for Siemens products is CISS (Constructive Interference Steady State). In this sequence, the fat and liquid signal is enhanced, making it possible to clearly differentiate surrounding structures even if they are submillimeter. This sequence is useful to study with precision the ventricular system, cisterns and venous sinuses, cranial nerves and CSF drainage [4-7].
The first line treatment must be in symptomatic patients the surgical excision of the lesion, but in few cases it is not technically possible so that fenestration and puncture aspiration of the cyst are the alternative therapy. The implantation of permanent bypass valves is reserved for recurring cases [8].
Conflict of interest and ethical statement
The authors have no conflicts of interest directly relevant to the content of this article. All authors have been personally and actively involved in substantive work leading to the manuscript. We respect the confidentiality an anonymity of the patient.
- Pereda GA, Ron AG, Martinez GM, Echevarría EM (2014) Procesos ocupantes de espacio no neoplasicos. In: Verdú Pérez A, ed. by. Manual de Neurología Infantil. 2nd ed. Madrid: Médica Panamericana 536-547.
- Vlaho S, Gebhardt B, Gerlach R, Weidauer S, Kieslich M (2003) Cyst of the third ventricle as an unusual cause of acquired hydrocephalus. Pediatr Neurol 28: 225-227. Link: http://bit.ly/2mfUUo1
- Chheda GM, Wen PY (2019) Uncommon brain tumors. Link: http://bit.ly/2lSJHd6
- Li Z, Chen YA, Chow D, Talbott J, Glastonbury C, et al. (2019) Practical applications of CISS MRI in spine imaging. Eur J Radiol Open 6: 231-242. Link: http://bit.ly/2lRLTl9
- Haridas A, Tomita T (2019) Hydrocephalus in children: Clinical features and diagnosis. Link: http://bit.ly/2kEmMC6
- Hingwala D, Chatterjee S, Kesavadas C, Thomas B, Kapilamoorthy T (2011) Applications of 3D CISS sequence for problem solving in neuroimaging. Indian J Radiol Imaging 21: 90. Link: http://bit.ly/2lSKURG
- Wang DD, Martin KW, Auguste KI, Sun PP (2015) Fast dynamic imaging technique to identify obstructive lesions in the CSF space: report of 2 cases. J Neurosurg Pediatr 15: 519-523. Link: http://bit.ly/2lTkwqK
- Ozek MM, Urgun K (2013) Neuroendoscopic Management of Suprasellar Arachnoid Cysts. World Neurosurg 79: S19.e13-e18. Link: http://bit.ly/2mmLCqF
Article Alerts
Subscribe to our articles alerts and stay tuned.
 This work is licensed under a Creative Commons Attribution 4.0 International License.
This work is licensed under a Creative Commons Attribution 4.0 International License.

 Save to Mendeley
Save to Mendeley
