Archives of Hematology Case Reports and Reviews
Coronavirus Disease 2019 (COVID-19)- Associated central retinal vein occlusion: A case report and literature review
Mohammad Hassan Hodroj1, Ziad F Bashshur2, Charbel Wahab2, Kawthar Jarrah3 and Ali Taher1,3*
2Department of Ophthalmology, American University of Beirut Medical Center, Beirut, Lebanon
3Division of Hematology and Oncology, Department of Internal Medicine, American University of Beirut Medical Center, Beirut, Lebanon
Cite this as
Hodroj MH, Bashshur ZF, Wahab C, Jarrah K, Taher A (2022) Coronavirus Disease 2019 (COVID-19)- Associated central retinal vein occlusion: A case report and literature review. Arch Hematol Case Rep Rev 7(1): 009-012. DOI: 10.17352/ahcrr.000037Copyright License
© 2022 Hodroj MH, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.Coronavirus Disease 2019 (COVID-19) is caused by the Severe Acute Respiratory Syndrome Coronavirus 2(SARS-CoV-2) that is associated with several inflammatory and vascular endothelial complications. Ocular vascular occlusive events were reported in COVID-19 patients including both Central Retinal Vein Occlusion (CRVO) and Central Retinal Artery Occlusion (CRAO). We report a case of a 34-years-old patient with right CRVO after 14 days of COVID-19 infection presenting with decreased vision. In addition, we provide a summary of both CRVO and CRAO reported in the literature.
Introduction
Late in December 2019, a novel coronavirus was identified to be responsible for unidentified pneumonia outbreaks and sporadic human infections. The virus was labeled as SARS-CoV-2 causing COVID-19 which was declared by the World Health Organization (WHO) as a pandemic in March 2020 affecting millions of people worldwide [1]. COVID-19 has been associated with different types of complications mainly vascular in nature where retinal occlusive vascular events, both venous and arterial were described and reported [2].
In this manuscript, we describe a case of central retinal vein occlusion in a 34-year-old male in the settings of COVID-19 infection. In addition, we review and summarize the reported cases of COVID-19 associated retinal occlusive vascular events in the literature.
Case report
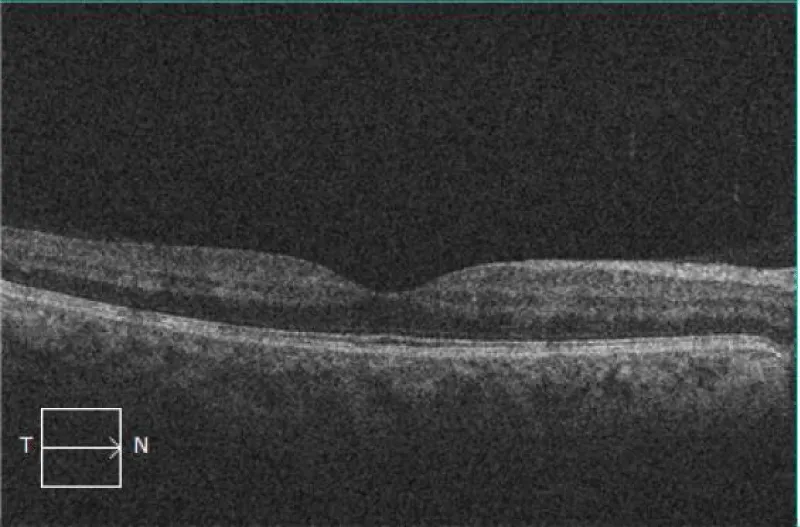
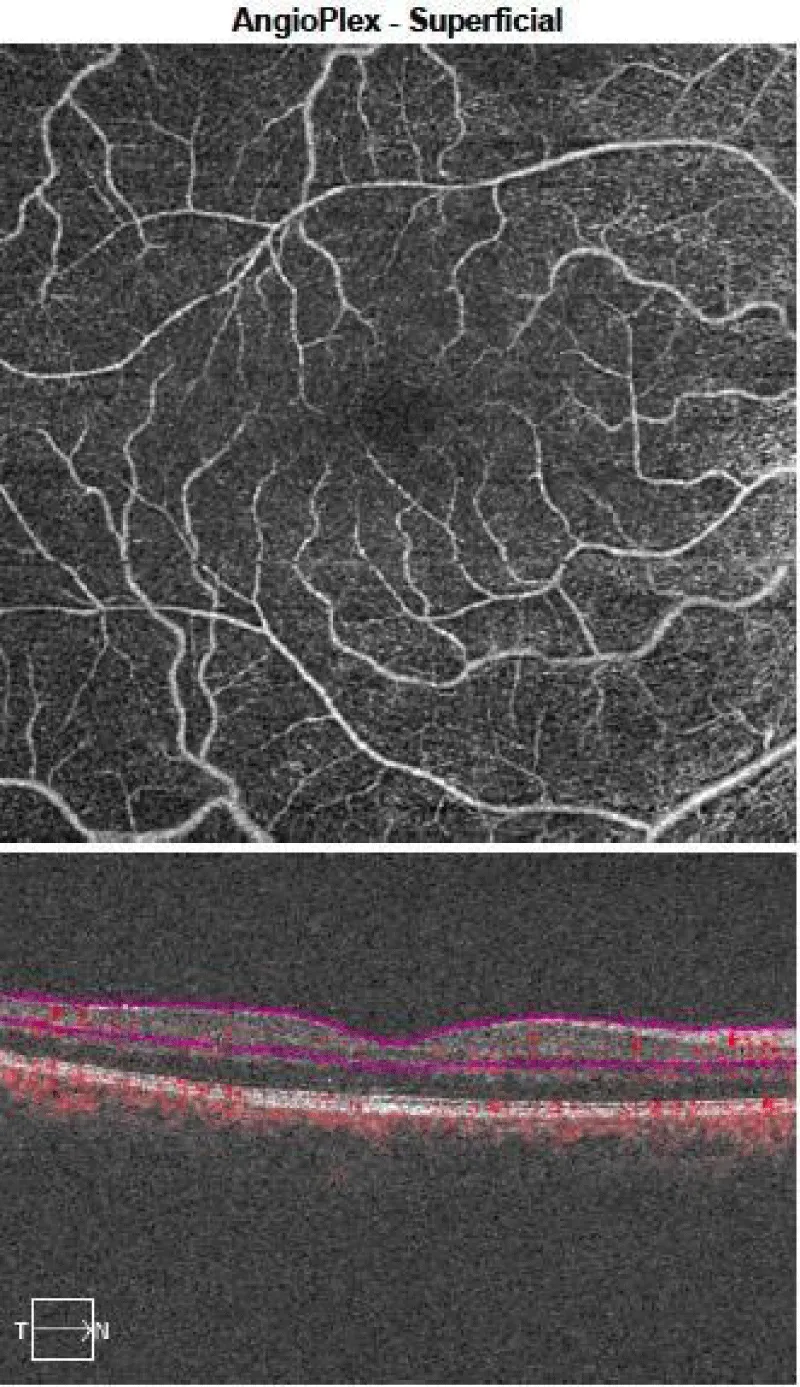
A 34-year-old male with type 1 diabetes mellitus since the age of 8 years on exogenous insulin, currently 55 International units (IU)/day, with controlled Hemoglobin bA1c and no previous ocular history (no previous diabetic retinopathy on previous ocular exams) developed fever and cough and tested positive for SARS-CoV-2 by Reverse Transcriptase-Polymerase Chain Reaction (RT-PCR) assay with mild pneumonia on chest imaging. The patient blood glucose level remained stable and well-controlled on the same insulin dose without the need for any changes. His symptoms were very mild for which he received only supportive treatment until symptoms resolved. Two weeks following the positive test, the patient presented with sudden decreased visual acuity and distorted vision in the right eye. In the clinic, his visual acuity was 20/20 in both eyes and the right and left intraocular pressures were 19 mmHg and 18mmHg respectively. Slit-lamp examination of the anterior segment was normal bilaterally. Similarly, dilated fundus examination of the left eye was unremarkable. However, the fundus of the right eye showed diffuse intra-retinal hemorrhages, retinal vein tortuosity and dilatation typical for (CRVO), but no evidence of macular edema. Optical Coherence Tomography (OCT) of the right eye was normal with a central retinal thickness of 247µm (Figure 1). Optical Coherence Tomography Angiography (OCTA) was done and showed no neovascularization (Figure 2).
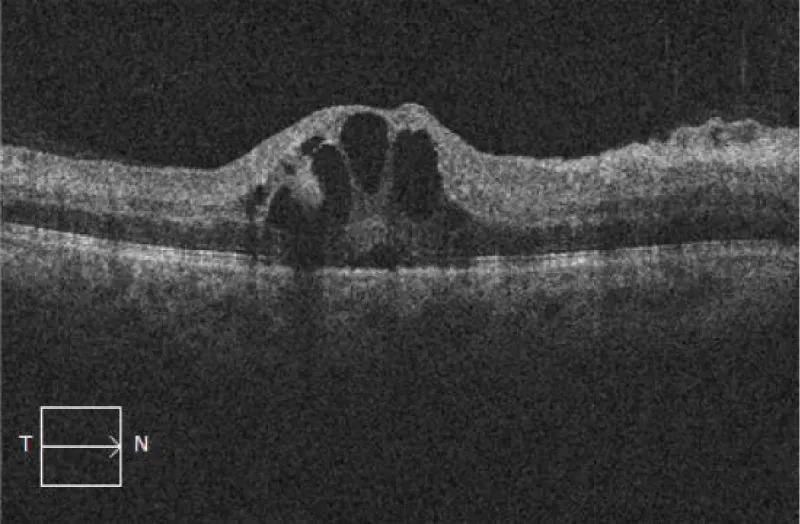
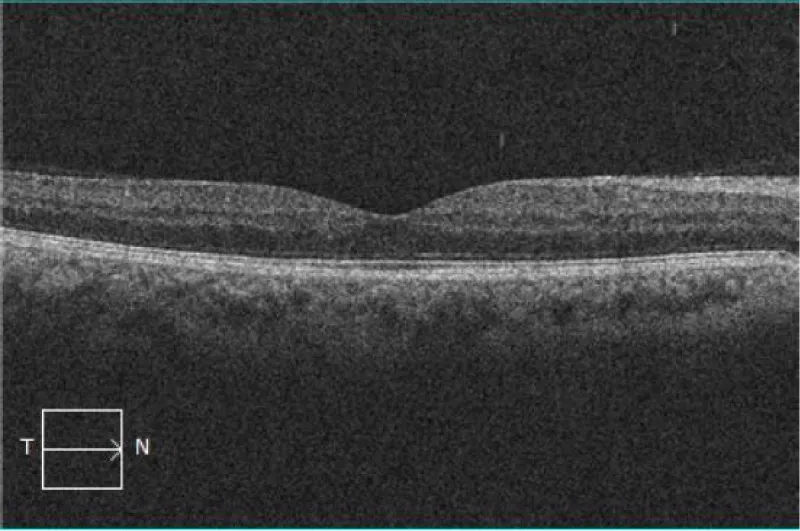
Diagnostic workup blood pressure, complete blood count, lipid panel, Hemoglobin bA1c, glucose level, C-reactive protein, erythrocyte sedimentation rate, anti-cardiolipin, lupus anti-coagulant, B2 glycoprotein 1 IgM and IgG antibodies, homocysteine and thrombophilia panel were unremarkable. The patient has no family history of thrombophilia and thrombosis. Based on what as mentioned above the patient was diagnosed with right central retinal vein occlusion and was followed up with monitoring. One month later, he reported worsening of his decrease in vision in the right eye with visual acuity of 20/25 and his repeat OCT showed the appearance of Cystoid Macular Edema (CME) with associated mild subretinal fluid (Figure 3) for which he was started on intravitreal antivascular endothelial growth factor (anti-VEGF) injections of aflibercept. One a month after the initiation of the injection, his visual acuity improved in the right eye to 20/20, and his OCT showed resolution of the macular edema (Figure 4).
Discussion
Retinal vein occlusion is a retinal vascular condition characterized clinically by engorgement, dilatation and tortuosity of retinal blood vessels that can progress if not treated into macular edema, intra-retinal bleedings, ischemic retinal areas, optic disc swelling, and reduced visual acuity.
Several medical conditions including hypertension, diabetes, vasculitis, and thrombophilia are the most common factors to be associated with retinal vascular events [3]. COVID-19-associated coagulopathy and hypercoagulability have been documented and investigated since the onset of the pandemic, demonstrating hallmark diffuse small vessel thrombosis and vascular endothelial lesions induced mainly by inflammation [4].
Hypercoagulability is a major risk factor for CRVO and it is essential to rule out other causes of CRVO in an otherwise healthy patient. Our patient is young and his diabetes is well controlled, with negative hypercoagulable studies which are similar to many of the reported cases in the literature [5]. In addition, it was shown that COVID-19 can cause a hyperinflammatory state that induces an increased risk of Venous Thromboembolism (VTE) in different sites and organs. However, the accurate mechanism is still not fully understood [4]. COVID-19 is believed to induce CRVO through either a VTE or by promoting retinal vasculitis secondary to thrombo-inflammatory cascade due to a cytokine-storm immune response through the excessive secretions of cytokines and chemokines by antigen-presenting cells and T-cells. Both mechanisms can lead to endothelial cell dysfunction and breakdown in the inner blood-retinal barrier leading to the development of macular edema due to increased capillary permeability [6]. Macular edema secondary to CRVO has been treated with different modalities in the literature. The use of intraocular steroids, systemic steroids and even antiplatelet medications were reported. However, as in our case, the most common treatment that is currently used is via blocking intraocular VEGF by injecting intravitreal anti-VEGF agents such as aflibercept, bevacizumab or ranibizumab [6,7].
Reviewing the literature, we found multiple articles reporting cases of COVID-19-associated CRVO; however, only 8 cases reported documented CRVO, 5 of whom are males and 3 are females with a period of time between COVID-19 symptoms and ocular symptoms ranging from 5 to 21 days except for one case of 60 days by Sanchez, et al. and an unknown period by Venkatesh, et al. as shown in (Table 1). Moreover, the first possible case of COVID-19 vaccine-induced non-ischemic CRVO was reported [8].
CRVO was not the only ocular vascular event in COVID-19, where central retinal artery occlusion (CRAO) was also documented in the settings of COVID-19 infection. CRAO is an ophthalmic an emergency that resembles myocardial infarctions to cardiologists and strokes to neurologists where the outcome can be a permanent vision loss [9]. CRAO was correlated with the predisposition to arterial thrombosis where the inflammatory state in COVID-19 induced changes in homeostasis leading to thrombotic disease in the arterial system as well as in the venous circulation [10].
Moreover, the available treatments of CRAO and their efficacies are still controversial and they include the use of thrombolytic agents and maneuvers such as ocular massage, use of intraocular hypotensive agents and anterior chamber paracentesis to dislodge the blood clot [9]. While a significant visual improvement is expected and observed with CRVO post-treatment, the visual recovery after CRAO is often very poor due to the lack of a definitive therapy [11]. Six cases of COVID-19-associated CRAO were reported and are summarized in (Table 2).
Conclusion
We present this interesting case of COVID-19-associated CRVO in order to shed the light on one of the emerging vascular complications of this disease. It was shown that COVID-19 infection can affect the vascularity of any organ through its hypercoagulability and hyperinflammatory state. In addition, we discussed the presence of CRAO and the current possible treatments of both entities.
This helps the physicians dealing with COVIID-19 patients to manage complications and to follow up closely on any ocular manifestations based on the reported durations for early diagnosis and appropriate management leading to better outcomes.
- Al Mahmasani L, Hodroj MH, Finianos A, Taher A (2021) COVID-19 pandemic and transfusion medicine: the worldwide challenge and its implications. Ann Hematol 100: 1115-1122. Link: https://bit.ly/35Ds3ku
- Cuadros Sánchez C, Egüen CS, Gutierrez-Ezquerro R, Giralt-Peret L, Fonollosa A (2021) Central Retinal Vein Occlusion Presumably Associated with Lupus Anticoagulant Induced by SARSCoV-2. Ocul Immunol Inflamm 1-4. Link: https://bit.ly/3K58nVA
- Gaba WH, Ahmed D, Al Nuaimi RK, Dhanhani AA, Eatamadi H (2020) Bilateral Central Retinal Vein Occlusion in a 40-Year-Old Man with Severe Coronavirus Disease 2019 (COVID-19) Pneumonia. Am J Case Rep 21: e927691. Link: https://bit.ly/3K58oZE
- Raval N, Djougarian A, Lin J (2021) Central retinal vein occlusion in the setting of COVID-19 infection. J Ophthalmic Inflamm Infect 11: 10. Link: https://bit.ly/3vz1jwt
- Sheth JU, Narayanan R, Goyal J, Goyal V (2021) Response to comments on: Retinal vein occlusion in COVID-19: A novel entity. Indian J Ophthalmol 69: 195-196. Link: https://bit.ly/3IBreHw
- Venkatesh R, Reddy NG, Agrawal S, Pereira A (2021) COVID-19-associated central retinal vein occlusion treated with oral aspirin. BMJ Case Rep 14: e242987. Link: https://bit.ly/3hv6mpa
- Rhoades W, Dickson D, Nguyen QD, Do DV (2017) Management of macular edema due to central retinal vein occlusion - The role of aflibercept. Taiwan J Ophthalmol 7: 70-76. Link: https://bit.ly/36WtpYh
- Endo B, Bahamon S, Martínez-Pulgarín DF (2021) Central retinal vein occlusion after mRNA SARS-CoV-2 vaccination: A case report. Indian J Ophthalmol 69: 2865-2866. Link: https://bit.ly/3IKiz5i
- Acharya S, Diamond M, Anwar S, Glaser A, Tyagi P (2020) Unique case of central retinal artery occlusion secondary to COVID-19 disease. IDCases 21: e00867. Link: https://bit.ly/3swDIKN
- Montesel A, Bucolo C, Mouvet V, Moret E, Eandi CM (2020) Case Report: Central Retinal Artery Occlusion in a COVID-19 Patient. Front Pharmacol 11: 588384. Link: https://bit.ly/3C0Rfxr
- Ucar F, Cetinkaya S (2021) Central retinal artery occlusion in a patient who contracted COVID-19 and review of similar cases. BMJ Case Rep 14: e244181. Link: https://bit.ly/35GbCUf
- Walinjkar JA, Makhija SC, Sharma HR, Morekar SR, Natarajan S (2020) Central retinal vein occlusion with COVID-19 infection as the presumptive etiology. Indian J Ophthalmol 68: 2572-2574. Link: https://bit.ly/3M9OIph
- Yahalomi T, Pikkel J, Arnon R, Pessach Y (2020) Central retinal vein occlusion in a young healthy COVID-19 patient: A case report. Am J Ophthalmol Case Rep 20: 100992. Link: https://bit.ly/3K8Ov3A
- Rego Lorca D, Rouco Fernandez A, Jimenez Santos M, Saenz-Frances F, Burgos-Blasco B, et al. (2021) Bilateral retinal vein occlusion and diabetic retinopathy after COVID-19. Acta Ophthalmol 99: e1246-e1248. Link: https://bit.ly/35fucmC
- Alam S, Dharia RN, Miller E, Rincon F, Tzeng DL, et al. (2021) Coronavirus Positive Patients Presenting with Stroke-Like Symptoms. J Stroke Cerebrovasc Dis 30: 105588. Link: https://bit.ly/3pqZ4Hz
- Bapaye MM, Nair AG, Bapaye CM, Bapaye MM, Shukla JJ (2021) Simultaneous Bilateral Central Retinal Artery Occlusion following COVID-19 Infection. Ocul Immunol Inflamm 29: 671-674. Link: https://bit.ly/3pqZ4Hz
- Larochelle R, Koduri V, Chen R, Subramanian PS (2021) Embolic abducens palsy and central retinal artery occlusion in a patient with COVID-19. J Neuroophthalmol. Link: https://bit.ly/36H0A1A

Article Alerts
Subscribe to our articles alerts and stay tuned.
 This work is licensed under a Creative Commons Attribution 4.0 International License.
This work is licensed under a Creative Commons Attribution 4.0 International License.
 Save to Mendeley
Save to Mendeley
