Archives of Hematology Case Reports and Reviews
A Patient Diagnosed with POEMS Syndrome with Atypical Presentation
Seyin Semiz H1*, Sarıkaya O1, Duran M2, Ozsan N3 and Saydam G2
2Faculty of Medicine, Department of Hematology, Ege University, Izmir, Turkey
3Faculty of Medicine, Department of Pathology, Ege University, Izmir, Turkey
Cite this as
Semiz HS, Sarıkaya O, Duran M, Ozsan N, Saydam G (2018) A Patient Diagnosed with POEMS Syndrome with Atypical Presentation. Arch Hematol Case Rep Rev 3(1): 001-003. DOI: 10.17352/ahcrr.000011Introduction
POEMS syndrome is a paraneoplastic syndrome due to an underlying plasma cell neoplasm. The major criteria for the syndrome are polyradiculoneuropathy, clonal plasma cell disorder (PCD), sclerotic bone lesions, elevated vascular endothelial growth factor, and the presence of Castleman disease. Minor features include organomegaly, endocrinopathy, characteristic skin changes, papilledema, extravascular volume overload, and thrombocytosis [1]. Autologous Stem Cell Transplantation (ASCT) might be potential approach of choice in patients that are eligible; otherwise, systemic therapies adopted from the therapeutic armamentarium for multiple myeloma are alternatives [2]. İn this paper, we reported that a patient which was treated with VAD (Vincristine, Doxorubicin, Dexamethasone 40 mg) with exlusion of vincristine due to existing neuropathy and ASCT with high-dose melphalan and improved; although the bone marrow biopsy did not observe a plasma cell clone.
Case Description
41 years old Caucasian female patient admitted to the hospital with the loss of sense in her hands and skin hyperpigmentation for 6 months. In her history, she had preeclampsia (13 years ago), hypertension (for 13 years) and no history of surgery with normal family history. Her hypertension has been treated and controlled with amlodipin 5 mg/day. During physical examination; hyperpigmentation, decreased lung sounds, low-volume heart sounds, hepatosplenomegaly, multiple axillary-inguinal lymphadenopathies, bilateral pretibial edema, quadriparesia and loss of the deep tendon reflexes in all extremities were noticed and recorded. Her muscle strength was 3/5 on upper extremities and 2/5 on lower extremitities, Laboratory analyses revelaed that; WBC: 12040 /uL (3040-9640/uL), Hb: 13, 3 g/dl (10, 8-14, 9), PLT: 676000/uL (150000-400000/uL), Urea: 65 mg/dl (0-38 mg/dl), Cr: 1.38 mg/dl (0, 5-0, 9 mg/dl) Uric Acid: 11.8 mg/dl ( 3, 4-7 mg/dl), Blood electrolytes: normal, LFT(Liver Function Tests): normal, Albumin: 3.7 g/dl (3, 4-4, 8 g/dl) , Globulin: 5 g/dl (2, 5-3, 5g/dl) ,LDH: 313 U/L (135-225 U/L) , CRP: 0.4 mg/dl (normal 0-0, 5mg/dl), ESR: 56mm/hour (normal 0-20mm/hour), fT3: 1,85 pg/ml (2-4, 4 pg/ml), fT4: 0, 74 ng/dl (0.93-1,7 ng/dl), TSH: 5.19 ng/dl (0,27-4,2 ng/dl). Urine analysis was normal and no proteinuria was detected. Chest X-ray showed the presence of bilateral pleural effusion as illustrated in figure 1.
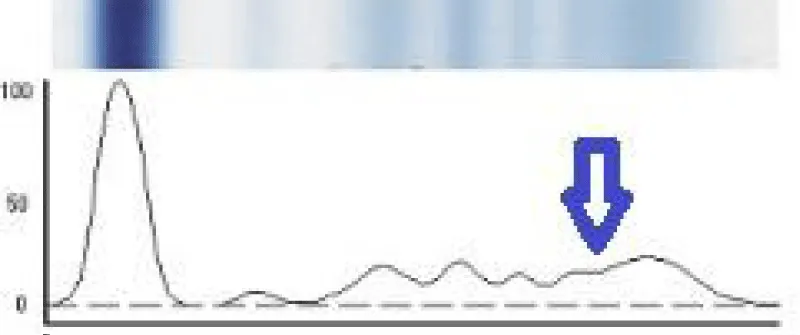
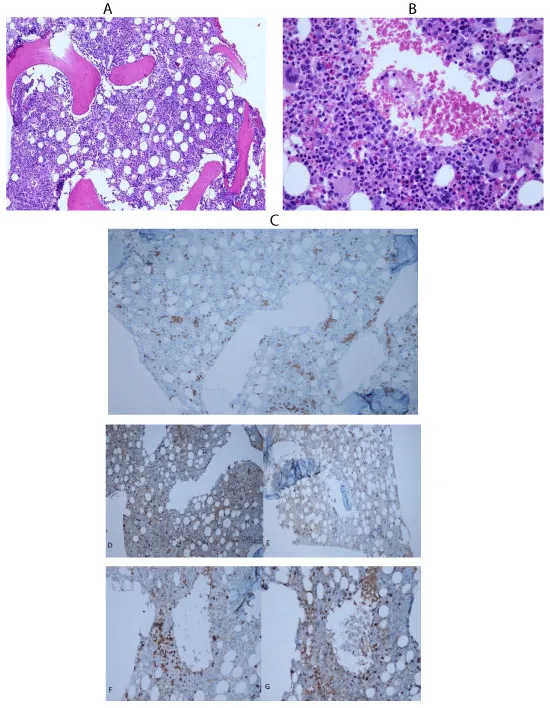
Abdominal USG confirmed the hepatosplenomegaly. Thoracoabdominal CT was performed and showed hepatomegaly, in the para-aortic area and inguinal area multiple bilateral lymph nodes, diffuse free fluid in the peritoneal, pericardial areas, bilateral pleural effusion, benign and reactive-looking multiple lymph nodes in both axillary areas. Peripheral blood smear has nothing special but thrombosytosis. Electromyography (EMG) was reported as demyelination and secondary axonal sensorimotor polyneuropathy Echocardiography (ECO) was reported as insufficiencies in mitral and tricuspid leaflets, ,mild pulmonary hypertension, and pericardial effusion. For differential diagnosis of lymphoproliferative disorders, we have performed fine needle aspiration from axillary lymph node and it was reactive. Due to high ESR and globulin levels, we have analyzed immunoglobulin levels. The results were as follows; IgA: 524 mg/dl (45-380 mg/dl), IgM : 156 mg/dl (40-230 mg/dl), IgG: 1390 mg/dl (650 – 1600 mg/ dl) Free light chain kappa(κ): 9.12 mg/dl ( 0.67 - 2.24 mg/ dl ), Free light chain lambda (λ): 27.6 mg/dl (0.83 - 2.7 mg/dl), Free light chain κ/λ ratio: 0.33 (0.31 - 1.56). Beta-2 microglobulin: 10271 ng/mL (651 – 2295 ng/mL), immunfixatiton electrophoresis and protein electrophoresis revealed that there was IgA lambda monoclonal gammopathy and beta gamma monoclonal band respectively (Figure 2). Unfortunately, in this case, the serum level of the vascular endothelial growth factor (VEGF) was not assessed.Bone marrow aspiration and biopsy were performed but revealed as normal with normal percentaged of plasma cells (Figures 3).
Since the patient has neuropathy, monoclonal gammopathy, endocrinopathy, organomegaly and skin changes, the diagnosis was accepted as POEMS syndrome and therapy was started. She was treated with VAD (Vincristine, Doxorubicin, Dexamethasone 40 mg) with exlusion of vincristine due to existing neuropathy and ıt was decided to perform ASCT with high-dose melphalan. ASCT was succesfully performed and the patient recovered quickly. 2 months later from ASCT, she started to walk and muscle weakness improved. She had been under follow up since two years and she had been very well. But last month she admitted our emergency service because of cuough since one month and progressive dyspnea . ECO releaved that; 1 cm pericardial effusion, tricuspid insufficiency 3rd degree, left ventricle(LV) diastolic disfunction (stage I), right ventricle (RV) systolic function moderate depressıon right ventricle ejection fraction(RVEF) 40% systolic pulmonary artery pressure (sPAP): 80 mmhg. She was interned to the intensive care unit of cardiology; becasue of severe pulmonary hypertension. While her treatment was contiuning, she had pneumonia and septic shock, then she died after one month.
Discussion
POEMS syndrome is a paraneoplastic syndrome due to an underlying plasma cell neoplasm. The major criteria for the syndrome are polyradiculoneuropathy, clonal plasma cell disorder (PCD), sclerotic bone lesions, elevated vascular endothelial growth factor, and the presence of Castleman disease. Minor features include organomegaly, endocrinopathy, characteristic skin changes, papilledema, extravascular volume overload, and thrombocytosis. Diagnoses are often delayed because the syndrome is rare and can be mistaken for other neurological disorders, most commonly chronic inflammatory demyelinating polyradiculoneuropathy. POEMS syndrome should be distinguished from the Castleman disease variant of POEMS syndrome, which has no clonal PCD and typically little to no peripheral neuropathy but has several of the minor diagnostic criteria for POEMS syndrome [1]. The diagnosis of POEMS syndrome should be based on 3 of the major criteria, two of which must include polyradiculoneuropathy and clonal plasma cell disorder, and at least one of the minor criteria (Table 1).
Diagnosis requires the mandatory presence of two major criteria plus at least one minor criterion [1]
As the pathogenesis of the syndrome is not well understood, risk stratification is limited to clinical phenotype rather than specific molecular markers. The number of clinical criteria is not prognostic, but the extent of the plasma cell disorder is. Those patients with an iliac crest bone marrow biopsy that does not reveal a plasma cell clone are candidates for local radiation therapy; those with a more extensive or disseminated clone will be candidates for systemic therapy. For those patients with a dominant sclerotic plasmacytoma, first-line therapy is irradiation. Patients with diffuse sclerotic lesions or disseminated bone marrow involvement and for those who have progression of their disease 3–6 months after completing radiation therapy should receive systemic therapy. Corticosteroids are temporizing, but alkylators are the mainstay of treatment, either in the form of low-dose conventional therapy or high dose with stem cell transplantation [3].
In our case, although the bone marrow biopsy did not observe a plasma cell clone, she was treated with VAD (Vincristine, Doxorubicin, Dexamethasone 40 mg) with exlusion of vincristine due to existing neuropathy and ıt was decided to perform Autologous Stem Cell Transplantation (ASCT) with high-dose melphalan. ASCT was succesfully performed and the patient recovered quickly. 2 months later from ASCT, she started to walk and muscle weakness improved. But she died after two years because of severe pulmonary hypertension. Pulmonary hypertension can be a clinical manifestation of POEMS syndrome in this patient. Because before the ASCT, her ECO had releaved the mild pulmonary hypertension. Pulmonary manifestations of POEMS syndrome include pulmonary hypertension (PH), which has been reported to occur in 27% of unselected patient with POEMS syndrome [3]. PH improved with treatment of the underlying plasma cell disorder in 88% of individuals undergoing either medical therapy including melphalan and steroids or autologous transplant [3,4]. Reversibility of pulmonary hypertension was observed after treatment of POEMS syndrome. After median follow of 32 months, survival of patients with pulmonary hypertension was worse than those without (median overall survival 54 months vs. median not reached, P=0.021). Although active treatment of POEMS syndrome can reverse pulmonary hypertension, survival of these patients is worse than those without pulmonary hypertension [5].
As a result; POEMS syndrome is a rare paraneoplastic plasma-cell disorder with myriad clinical manifestations which are often subtle and overlooked by clinicians in early stages. ASCT might be potential approach of choice in patients that are eligible; otherwise, systemic therapies adopted from the therapeutic armamentarium for multiple myeloma are alternatives [2]. Patients with POEMS syndrome undergoing to an autologous peripheral blood stem cell transplant (PBSCT) have very high and long lasting responses. At present ASCT should be considered as the first line therapy in young patients with POEMS, eligible for high dose melphalan, in the absence of organ dysfunction [6]. As an exception to our case; although the patient had normal plasma cells in the bone marrow biopsy, she responded to the ASCT but she died after two years because of severe pulmonary hypertension.
- Jeunon T, Sampaio AL, Caminha RC, Reis CU, Dib C (2011) Glomeruloid hemangioma in POEMS syndrome: a report on two cases and a review of the literature. An Bras Dermatol 86: 1167-1173. Link: https://tinyurl.com/yalljsnp
- Warsame R, Yanamandra U, Kapoor P (2017) POEMS Syndrome: an Enigma. Curr Hematol Malig Rep 12: 85–95. Link: https://tinyurl.com/yb8jr7lm
- Dispenzieri A (2017) POEMS syndrome: 2017 Update on diagnosis, risk stratification, and management. Am J Hematol 92: 814–829. Link: https://tinyurl.com/yacx2ea3
- Chandrashekaran S, Dispenzieri A, Cha SS, Kennedy CC (2015) Pulmonary morbidity improves after autologous stem cell transplantation in POEMS syndrome. Respir Med 109: 122–130. Link: https://tinyurl.com/y7h8s968
- Li J, Tian Z, Zheng HY, Zhang W, Duan MH, et al. (2013) Pulmonary hypertension in POEMS syndrome. Haematologica 98: 393–398. Link: https://tinyurl.com/ya252mxa
- Autore F, Innocenti I, Luigetti M, Piccirillo N, Sora F, et al. (2017) Autologous peripheral blood stem cell transplantation and the role of lenalidomide in patients affected by poems syndrome. Hematol Oncol 36: 392-398. Link: https://tinyurl.com/ycypjhmj
Article Alerts
Subscribe to our articles alerts and stay tuned.
 This work is licensed under a Creative Commons Attribution 4.0 International License.
This work is licensed under a Creative Commons Attribution 4.0 International License.


 Save to Mendeley
Save to Mendeley
