Archives of Clinical Gastroenterology
Liver Necrosis and Hemorrhage due to Gastroduodenal Artery Pseudoaneurysm after total Pancreatectomy. Report of a case
Kurşat Rahmi Serin, Muharrem Oner and Nadir Adnan Hacım*
Cite this as
Serin KR, Oner M, Hacım NA. (2018) Liver Necrosis and Hemorrhage due to Gastroduodenal Artery Pseudoaneurysm after total Pancreatectomy. Report of a case. Arch Clin Gastroenterol 4(3): 032-034. DOI: 10.17352/2455-2283.000056Although mortality after pancreatectomy in high-volume centers is less than 3%, morbidity is still as high as 18-52%. Postpancreatectomy vasculary complication is less frequent but much mortal than anastomotic problems. Postpancreatectomy vasculary complication is a life-threatening entity and it must be managed urgently. Here we report a case treated with emergent laparotomy for delayed liver ischemia and massive bleeding after total pancreatectomy. Patient was discharged without any complication at the 3rd week of emergent laparotomy for aneurismatic hemorrhage.
Upper gastrointestinal bleeding in the late postoperative period following pancreatoduodenectomy should alert the surgeon to the possibility of a ruptured visceral vasculary pseudoaneurysm.
Introduction
The most commen causes of developing pseudoaneursym after visceral surgery are infection and the enzymatic contamination, especially after GI surgery [1]. A ruptured pseudoaneurism with bleeding into the gastrointestinal tract, pancreatic duct, retroperitoneum, or peritoneal cavity is still life-threatening condition and mortality rate is still more than 15% in the era of modern surgery and minimally invasive radiological procedures [2-4]. The development of pseudoaneursyms after upper abdominal surgery is rare and it especially occurs after biliary and pancreatic arcade constitue [5].
Case Report
Total pancreatectomy and splenectomy was performed for pancreatic adenocarcinoma in a 70 years-old man. He was discharged at the 7th day of the surgery without any complication but 2 days after discharged he readmitted to hospital with uneasiness, weakness and subfebrile fewer (37.5‘C). He had anemia in his laboratoury and leukocytosis. Upper GI endoscopy planned and bleeding from gastrojejunal anastomosis was seen. Bleeding stopped with endoscopic sclerotherapy. During his stay he had fever above 38’C, computed tomography was done to detect the intraabdominal problems. He had surgical area fluid collection with suspicious infection (not maturated abscess?) at the side of the pancreatic head. Parenteral antibiotics started and the infection was well-treated by this way without any abscess formation and he was discharged without any problem under oral antibiotics.
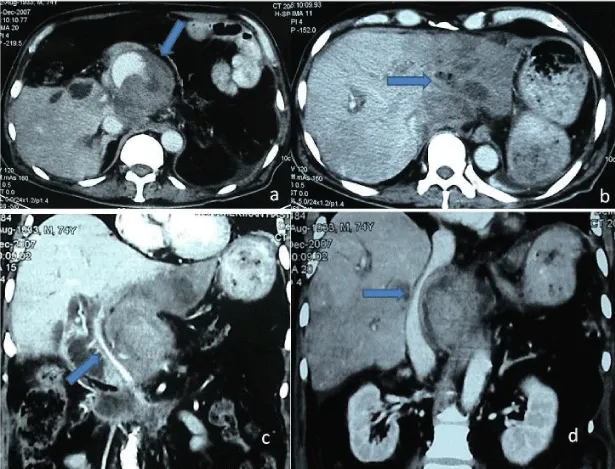
On the 30th day of the pancreatectomy he was readmitted to emergency department with fever complaint again. But his vital signs showed he was in shock, may be caused by sepsis. Computed tomography was performed urgently and gastroduodenal artery pseudoanevrism rupture and intraabdominal bleeding diagnosed. He had retroperitoneal hematoma that was compressing to vena cava inferior and portal vein. And the left hepatic lobe was ischemic (Figure 1). He was operated urgently, during the laparotomy he had mild bleeding in the abdominal cavity but he had ruptured gastroduodenal artery aneurism, app.10cm was seen. Arterial aneurismatic ruptured side was under compression by the hematoma without active massive bleeding. Gastroduodenal artery dissected and the trunk from the hepatic artery exposed and ligated. Hepatic artery doppler ultrasound confirmed the flow at the right side but there is no arterial flow at the left side. Portal vein left and right branches seen avoided but the left lobe of the liver was seen blue. Hemostasis after aneurismectomy provided. There is no fluid collection, abscess or any other surgical complication seen inside the abdomen. Patient taken to the theater under hemorrhagic shock with wicked general condition and due to damage control surgery procedure left liver left in this situation. In the 3rd day of the surgery he was taken to ward from ICU and liver ischemia was well-treated by conservative approach. The patient stayed alive without local or systemic recurrence of disease on the 14 months follow-up after the initial treatment.
Discussion
Bleeding complication after pancreatectomy can be seen rarely due to ruptured visceral vasculary pseudoaneurysms [2,4,5]. This rare but mortal complication usually necessitates emergent surgery [5]. Stabile et al. reported its mortality rate more than 43% [6]. Delayed diagnosis and difficulties are the major obstacles in this high mortality rate. Bleeding complication after pancreatectomy or major abdominal surgery is especially seen at the upper gastrointestinal tract or either at the anastomotic site, especially after anastomotic problems, this primarily suggest endoscopic procedure for diagnosis and moreover for the treatment. Therefore, it must be kept in mind that it is difficult to enter the afferent jejunal loop by endoscope to detect the bleeding site and mucosal erosions or intermittent bleeding can be misleading and even hazardous causing delay in definitive treatment [7-10]. In our case, in the early postoperative days he had mild bleeding from the anastomotic site which controlled by endoscopic sclerotherapy and he had surgical side infection. Later on, he had massive bleeding from the visceral vasculature that was necessitated surgery, might be caused by this endoscopic intervention and infection.
Gastroduodenal artery is the most commen site for pseudoanevrism developing after pancreatectomies especially after Whipple’s procedure. This is usually associated as a result of leakage from the pancreaticojejunal anastomosis which causes infection or damages arteries [7,8]. Pancreatic proteolitic enzymes and destruction of the vessel walls during the lymphatic dissection are discussed for the local arteritis [3,11-15]. Intraabdominal infection is found in the great majority of these patients. As a matter of fact, in our cases, early postoperative complaints and surgical findings were made us consider about infection but there is no chance for the leakage.
We didn’t use ultrasonography to detect bleeding especially in hemodinamically instable patients. Contrast-enhanced computerized tomography and CT angiography can distinguish intraabdominal bleeding and also pseudoaneurysms [9].
Over the past decades, visceral angiography has improved the diagnostic and also therapeutic accuracy for visceral pseudoaneurysms [5]. Embolization with coils or covered stent implantation (especially in hemodynamic stable patients) became the first choice treatment modality [5,12,13]. However, angiography may not be helpful in mild or intermittent bleeding for showing and treating the site [12]. Moreover, revascularization and recurrent bleeding are not rare after intravasculary treatments. Salam et al. reported 37% recurrent bleeding in their series [14]. We couldn’t perform angiography for neither diagnosis nor treatment because of the hemodynamically instability of the patient (he was in shock due massive bleeding and in the cause of infection) and due to the hospital set-up, also.
Surgical exploration at the early postoperative period is also difficult, due to dense adhesions and fibrosis caused by previous surgery and infection. Furthermore an intact anastomosis can be damaged during dissection of the aneurysmatic artery. Since ligation of the artery alone may be insufficient, a completion pancreatectomy seems more reasonable, especially in anastomotic leakage [6].
In conclusion, pseudoaneurysms must be kept in mind as a cause of massive hemorrhage in the late postoperative period after pancreatectomies, particularly in patients who had postoperative anastomotic leakage and infective complications.
- Cameron JL, Pitt HA, Yeo CJ, Lillemoe KD, Kaufman HS, et al. (1993) One hundred and forty-five consecutive pancreaticoduodenectomies without mortality. Ann Surg 217: 430-435. Link: https://tinyurl.com/yadzabxt
- Miedema BW, Sarr MG, van Heerden JA, Nagorney DM, McIlrath DC, et al. (1992) Complications following pancreaticoduodenectomy. Current management. Arch Surg 127: 945-949. Link: https://tinyurl.com/ycmyq8yl
- Bergert H, Hinterseher I, Kersting S, Leonhardt J, Bloomenthal A, et al. (2005) Management and outcome of hemorrhage due to arterial pseudoaneurysms in pancreatitis. Surgery 137: 323-328. Link: https://tinyurl.com/y79awdvl
- Trede M, Schwall G (1988) The complications of pancreatectomy. Ann Surg 207: 39-47. Link: https://tinyurl.com/yadeggk2
- Reber PU, Baer HU, Patel AG, Triller J, Büchler MW (1998) Life-threatening upper GI tract bleeding caused by ruptured extrahepatic pseudoaneurysm after pancreatoduodenectomy. Surgery 124: 114-115. Link: https://tinyurl.com/yc52cos8
- Stabile BE, Wilson SE, Debos HT (1983) Reduced mortality from bleeding pseudocysts and pseudoaneurysms caused by pancreatitis. Arch Surg 118: 45-51. Link: https://tinyurl.com/ya7r8ma7
- Otah E, Cushin BJ, Rozenblit GN, Neff R, Otah KEE, et al. (2002) Visceral artery pseudoaneurysms following pancreatoduodenectomy. Arch Surg 137: 55- 59. Link: https://tinyurl.com/ybbahbfg
- Reber PU, Baer HU, Patel AG, Triller J, Büchler MW (1998) Life-threatening upper GI tract bleeding caused by ruptured extrahepatic pseudoaneurysm after pancreatoduodenectomy. Surgery 124: 114-115. Link: https://tinyurl.com/yc52cos8
- Yeo CJ (1995) Management of complications following pancreatoduodenectomy. Surg Clin North Am 75: 913-920. Link: https://tinyurl.com/y7nm2zpq
- Brodsky JT, Turnbull ADM (1991) Arterial hemorrhage after pancreatoduodenectomy; the “sentinel” bleed. Arch Surg 12: 1037-1040. Link: https://tinyurl.com/yc5sqet9
- Otah E, Cushin BJ, Rozenblit GN, Neff R, Otah KEE, et al. (2002) Visceral artery pseudoaneurysms following pancreatoduodenectomy. Arch Surg 137: 55- 59. Link: https://tinyurl.com/ybbahbfg
- Aranha GV, O’Neil S, Borge MA (1999) Successful nonoperative management of bleeding hepatic artery pseuddoaneurysms following pancreatoduodenectomy. Dig Surg 16: 528-530. Link: https://tinyurl.com/y8m4wued
- Pasklinsky G, Gasparis AP, Labropoulos N, Pagan J, Tassiopoulos AK, et al. (2009) Endovascular covered stenting for visceral artery pseudoaneurysm rupture: report of 2 cases and a summary of the disease process and treatment options. Vasc Endovascular Surg 42: 601-606. Link: https://tinyurl.com/ycazzwwy
- Salam TA, Lundsden AB, Martin LG, Smith RB (1992) Nonoperative management of visceral aneurysms and pseudoaneurysms. Am J Surg 164: 215-219. Link: https://tinyurl.com/ya2tv6lo
- Sumimoto H, Kaneko T, Ishıguchi T, Takai K, Ohta T, et al. (2001) Delayed rupture of a pseudoaneurysms following pancreatoduodenectomy; report of a case. Surg Today 31: 932-935. Link: https://tinyurl.com/y848rsc4
Article Alerts
Subscribe to our articles alerts and stay tuned.
 This work is licensed under a Creative Commons Attribution 4.0 International License.
This work is licensed under a Creative Commons Attribution 4.0 International License.

 Save to Mendeley
Save to Mendeley
