Open Journal of Trauma
Premature Physeal Closure of an Extraphyseal Distal Radius Fracture Secondary to Smooth Kirschner Wire Fixation: A Case Report
Michael C Doarn* and Mark S Cohen
Cite this as
Doarn MC, Cohen MS (2018) Premature Physeal Closure of an Extraphyseal Distal Radius Fracture Secondary to Smooth Kirschner Wire Fixation: A Case Report. Open J Trauma 2(1): 001-004. DOI: 10.17352/ojt.000016Premature closure of the distal radius physis is rare and is usually associated with a fracture pattern that involves the physis. We present a case of an extraphyseal distal radius fracture treated with closed reduction and percutaneous smooth Kirschner wire fixation that went on to premature physeal closure at the site of wire fixation. Surgeons should be aware that closures of the distal radius physis after metaphyseal fractures can occur with use of smooth Kirschner wires and that patients should be followed closely.
Introduction
Distal radius fractures are common in the pediatric population [1]. The majority are physeal Salter-Harris type I or II patterns [2]. Extraphyseal fractures often occur and usually go on to union without complications.
Pediatric fractures of the distal radius that involve the physis have a risk of premature physeal arrest. This has been reported in the literature between 1 and 7% [1]. Salter-Harris type II patterns are reported as having the highest risk for physeal closure [3]. Risk factors include multiple attempts at closed reduction and reduction performed greater than 7-10 days from the injury [1,3]. Metaphyseal distal radius fractures that are extraphyseal can be associated with premature physeal closure. However, this is extremely rare. All six such reported cases involved complete closure presumably due to a concomitant Salter-Harris type V compression injury to the growth plate [4].
We report a case of a patient with an isolated extraphyseal distal radius fracture that developed a partial premature physeal closure after smooth Kirschner wire fixation was used. The closure occurred directly where the pins had crossed the growth plate. This ultimately required a complex corrective osteotomy with lengthening of the radius.
Presentation of the Case Report
An 11 year-old right-hand-dominant healthy male presented after sustaining an isolated injury to his right wrist while snowboarding two days prior. The patient was seen at an outside emergency room and a splint was applied without manipulation. On examination, he had a normal neurovascular exam and full digital motion. An obvious clinical deformity was present. Radiographs of the right wrist revealed an extra-articular, extra-physeal distal radius fracture with dorsal angulation.
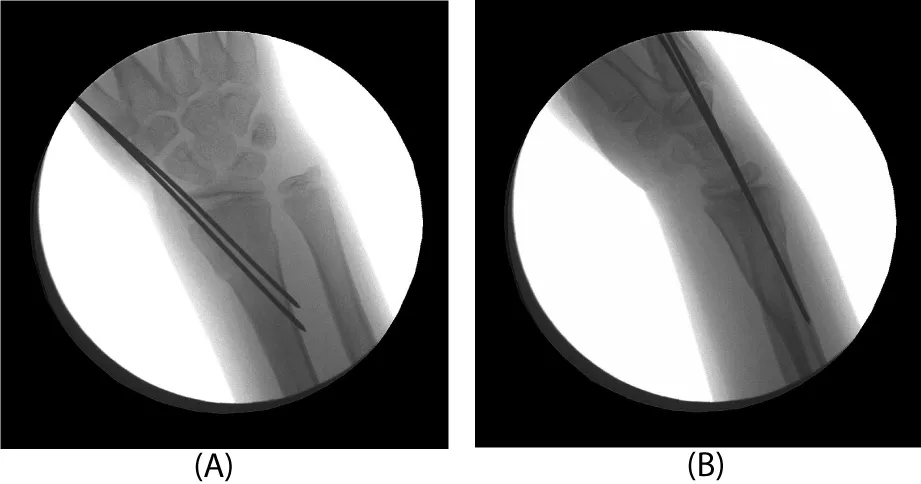
Three days after injury, consent was obtained, and the patient was taken to the operating room. There he underwent a manipulative closed reduction. Once reduction was obtained, percutaneous pin fixation was utilized to stabilize the fracture. Under flouroscopic guidance, two smooth 0.062 inch Kirschner wires were placed into the radial styloid tip and across the fracture site (Figure 2). Both pins were placed uneventfully with one attempted insertion. There were not multiple passes. The patient was then placed in a short arm cast that was split in the operating room.
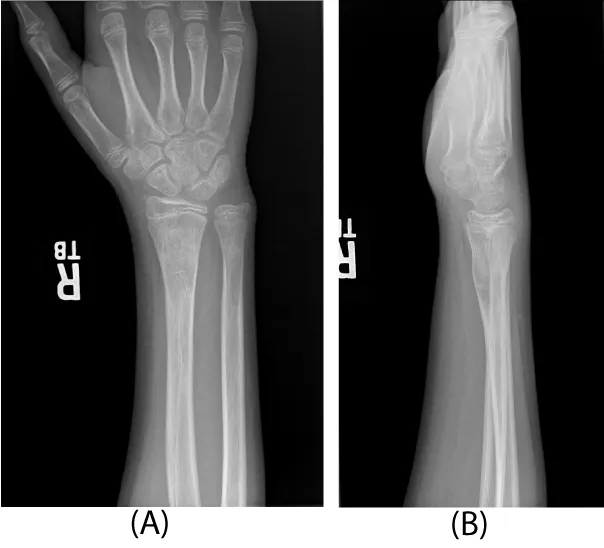
The patient remained immobilized in a short arm cast until 5 weeks post-operatively. At that time, he was taken back to the operating room for Kirschner wire removal. A post-operative splint was placed for one additional week. At that time, radiographs revealed complete healing of the fracture in adequate position and therapy was initiated. At twelve weeks post-operatively, the patient was noted to have full wrist mobility and he was allowed to progress with activity as tolerated. Radiographs revealed complete healing of the fracture and the physis appeared un-affected (Figure 3).
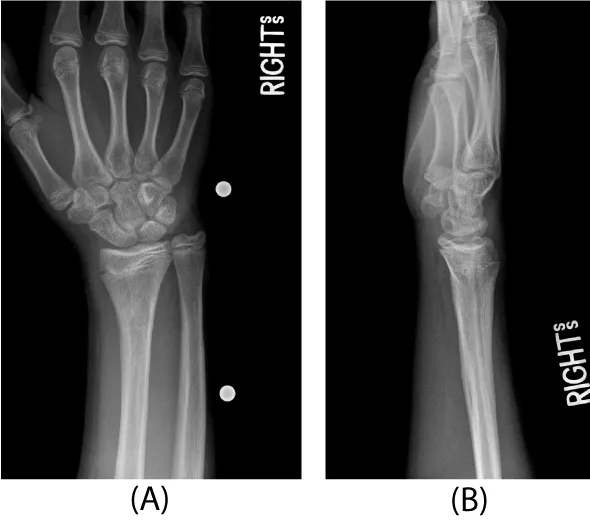
The patient returned two years later due to ulnar sided wrist pain. Clinical examination showed an obvious deformity with a prominent ulna and radial translation of the hand relative to the forearm axis. Radiographs revealed a partial distal radius physeal closure on the radial aspect where the original pins had been positioned. There was a reversal of the normal radial inclination on the frontal film and significant ulnar positive variance (Figure 4). The physis of the distal ulna remained open.
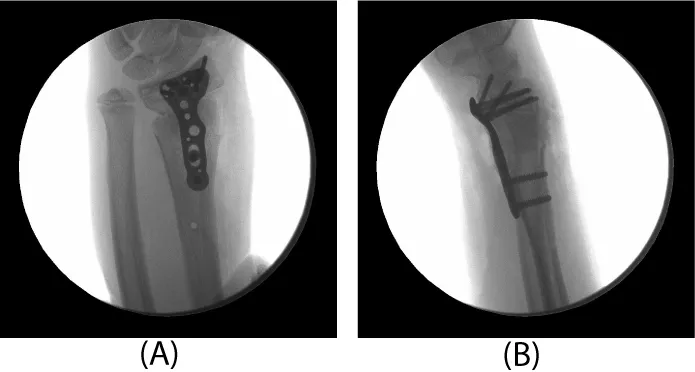
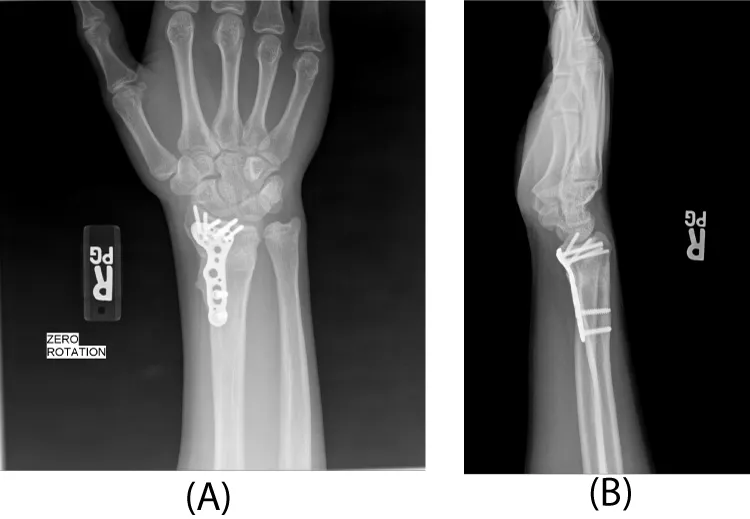
After pre-operative education and informed consent was obtained, the patient was taken back to the operating room for a complex distal radius osteotomy. Care was taken to recover radial length and realign the sigmoid notch of the distal radius relative to the head of the ulna at the distal radioulnar joint per the pre-operative plan and template. In order to recover length, the plate was first applied to the radius and then removed for the osteotomy. It was then reapplied to the distal fragment with locking screws. The plate was then reduced to the radial shaft proximally. Once length was obtained, the radius was secured to the radial shaft with a locking and a non-locking screw (Figure 5). The large trapezoidal metaphyseal defect was then filled with pure cancellous autograft obtained from the ipsilateral iliac crest (Figure 6). A 40mm acetabular reamer was used for this purpose, starting on the outer table and reaming toward, but not violating, the inner table. The remaining radial physis that remained open (ulnarly) was closed with a small burr under image control. The distal ulnar physis was similarly closed through a small ulnar incision to prevent further progression of growth mismatch (Figure 7). At 3 months following the osteotomy, radiographs showed complete healing with incorporation of the bone graft. In addition, the distal ulnar physis had closed. The patient regained full wrist range of motion with 75o extension, 90o flexion, 85o pronation and supination. This was symmetric with his contralateral side. His grip strength was 80 pounds bilaterally. He denied any pain or wrist symptoms and returned to sports and weightlifting. Final follow-up at one year revealed full mobility and symmetrical wrist and forearm motion (no measureable side to side differences). Radiographs showed maturation of the bone graft with remodeling (Figure 8).
Discussion
Disruption of distal radius physeal growth can occur from various etiologies including infection, ischemic conditions, and repetitive stress. Disruption is usually secondary to wrist trauma [1-5]. Closure of the radial growth plate occurs most commonly after Salter fractures which involve the physis. Other than this pattern, there have been six reported cases of pediatric extraphyseal metaphyseal fractures that developed premature closure. These cases were all treated non-operatively. In each case, the entire radial physis closed prematurely. The growth plate disturbance in these cases was attributed to a presumed concomitant crush injury to the distal radial physis that was unrecognized [2,4,6]. This is the first reported case that we are aware of involving a distal radius extraphyseal fracture treated with smooth Kirschner wire fixation complicated by premature physeal closure. In our patient, the growth plate closed with a bony bar on the radial side, exactly where the initial pins were placed. We thus believe that a concomitant Salter fracture to the radius is highly unlikely as these usually have complete physeal closure. We can only conclude that the bony bar was secondary to our surgical intervention.
Previous studies evaluating the effect of smooth pins placed across the physis have shown no significant risk to physeal growth [7,8]. However, most studies have involved the distal femoral physis. In addition, the location of the wires (centrally versus peripherally) has not been shown to be significant in animal models [8]. The exact cause of the bony bar from the pins in our case is thus not entirely clear. It is assuredly a rare complication.
Once physeal arrest occurs in the radius and affects wrist and forearm anatomy, including the distal radioulnar joint, various treatment options exist [9-12]. Patients can undergo a lengthening osteotomy of the radius, a shortening osteotomy of the ulna (typically with closure of the ulnar physis), or a combination of the two [1,10,11]. Due to the gross three dimensional deformity present in our patient with reversal of the normal radial inclination, we chose to realign the wrist and forearm by correcting the radius alone. While an additional shortening of the ulna could have been considered, we found this not to be necessary intra-operatively. In addition, we did close the remaining physis of the radius and that of the ulna.
With the significant lengthening of the radius, a very large trapezoidal defect remained. We chose to fill this with non-structural bone graft, rather than a more traditional corticocancellous bone block. This was facilitated by the use of a locking plate, which maintained the three-dimensional anatomy of the reduction during healing.
In conclusion, we believe that adolescents with distal radius fractures that are treated with pin fixation, regardless of whether the fracture involves the growth plate or not, should be followed with surveillance radiographs to document normal growth and alignment of the wrist for at least one year after surgery. In this way, early growth plate disturbances might be identified before a significant deformity occurs that might require a corrective radius osteotomy as seen in our patient.
- Abzug JM, Little K, Kozin SH (2014) Physeal arrest of the distal radius. J Am Acad Orthop Surg 22: 381-389. Link: https://goo.gl/1wVShm
- Cannata G, De Maio F, Mancini F, Ippolito E (2003) Physeal fractures of the distal radius and ulna: long-term prognosis. J Orthop Trauma. 17: 172-180. Link: https://goo.gl/zZtWxy
- Valverde JA, Albiñana J, Certucha JA (1996) Early posttraumatic physeal arrest in distal radius after a compression injury. J Pediatr Orthop B. 5: 57-60. Link: https://goo.gl/tjMYo7
- Tang CW, Kay RM, Skaggs DL (2002) Growth arrest of the distal radius following a metaphyseal fracture: case report and review of the literature. J Pediatr Orthop B 11: 89-92. Link: https://goo.gl/gNy8Av
- Birch JG, Herring JA, Wenger DR (1984) Surgical anatomy of selected physes. J Pediatr Orthop 4: 224-231. Link: https://goo.gl/6bC3kC
- Aminian A, Schoenecker PL (1995) Premature closure of the distal radial physis after fracture of the distal radial metaphysis. J Pediatr Orthop 15: 495-498. Link: https://goo.gl/BFd5qV
- Garrett BR, Hoffman EB, Carrara H (2011) The effect of percutaneous pin fixation in the treatment of distal femoral physeal fractures. J Bone Joint Surg Br 93: 689-694. Link: https://goo.gl/VHV8e4
- Dahl WJ, Silva S, Vanderhave KL (2014) Distal femoral physeal fixation: are smooth pins really safe? J Pediatr Orthop 34: 134-138. Link: https://goo.gl/4TjyAS
- Graham TJ (1997) Surgical correction of malunited fractures of the distal radius. J Am Acad Orthop Surg 5: 270-281. Link: https://goo.gl/9vbBG8
- Waters PM, Bae DS, Montgomery KD (2002) Surgical management of posttraumatic distal radial growth arrest in adolescents. J Pediatr Orthop 22: 717-724. Link: https://goo.gl/LrgCZn
- Kim BS, Song HS (2011) A comparison of ulnar shortening osteotomy alone versus combined arthroscopic triangular fibrocartilage complex debridement and ulnar shortening osteotomy for ulnar impaction syndrome. Clin Orthop Surg 3: 184-190. Link: https://goo.gl/Lc8sza
- Kang HG, Yoon SJ, Kim JR (2010) Resection of a physeal bar under computer-assisted guidance. J Bone Joint Surg Br 92: 1452-1455. Link: https://goo.gl/t2ZFJq
Article Alerts
Subscribe to our articles alerts and stay tuned.
 This work is licensed under a Creative Commons Attribution 4.0 International License.
This work is licensed under a Creative Commons Attribution 4.0 International License.



 Save to Mendeley
Save to Mendeley
