International Journal of Vascular Surgery and Medicine
Lower Extremity Venous Ablation as a Treatment Modality for Refractory Lichen Simplex Chronicus and Generalized Pruritus
Robert Wills DO, James Kleist, Hossein Akhondi* and Sassan Kaveh
Cite this as
Robert Wills DO, Kleist J, Akhondi H, Kaveh S (2018) Lower Extremity Venous Ablation as a Treatment Modality for Refractory Lichen Simplex Chronicus and Generalized Pruritus. Int J Vasc Surg Med 4(1): 001-003. DOI: 10.17352/2455-5452.000030Introduction: Lichen simplex chronicus (LSC) is a skin condition characterized by thick, leathery, scaly and extremely itchy patches of skin. It is a common pathology (up to 12% of population) with significant effect on quality of life without any established clear etiology or treatment.
Chronic venous insufficiency (CVI) is a progressive disease of the legs that occurs when the delicate bicuspid valves in the veins become weakened and develop reflux. CVI has been associated with many complications including local or generalized pruritus that may lead to intractable itch-scratch cycle, leading to LSC lesions on various parts of the body.
Cases: Recent development of multiple in-office ablation techniques for treatment of CVI have led to the added benefit of resolving the itch-scratch cycle, which in turn become the cure for LSC lesions. We present 6 cases with typical refractory LSC lesions whom we were able to cure after treatment of CVI using Radiofrequency ablation or Clarivein techniques.
Conclusion: We recommend all primary care physicians and dermatologists to consider an underlying CVI as a potential cause for any LSC lesions or even intractable pruritus.
Introduction
Lichen simplex chronicus (LSC) is essentially lichenified skin caused by repeated rubbing or scratching. Chronic scratching causes further itching through several mechanisms, creating a vicious cycle. LSC is commonly diagnosed by clinical presentation: thickened, leathery, scaly, hyperpigmented and excoriated. LSC lesions can involve any part of the body but typically starts in the medial aspects of the distal legs before spreading to the other parts. The itch usually starts in the evenings, but scratching happens in the middle of sleep and then progresses to a constant intractable itch that can very negatively impact quality of life.
The underlying etiology of LSC has been attributed to pruritic sequela of focal trauma. This lack of understanding and objective rational for the itch has led to the neurotic behavior hypotheses which implies anxiety and obsessive-compulsive disorder as the underlying cause. Hence the term Neurodermatitis is often used.
Treatment is commonly focused on relieving pruritus and skin manifestations, with the perception that LSC is a primary skin condition. Treatment recommendations vary from topical corticosteroids, injected corticosteroids, topical calcineurin inhibitors, antihistamines, gabapentin, Ultra Violate B, colloid baths, coal tar and behavioral modifications.
Chronic venous insufficiency (CVI) is a systemic disease that can have grave skin manifestations. These include not only LSC lesions but also stasis dermatitis and venous stasis ulcers. CVI can increase hydrostatic pressure, causing skin compromise and progression to local reaction due to release of inflammatory mediators. Other non-dermatological symptoms of CVI include leg ache, refractory edema, muscle cramps and restless legs. Physicians have recently been more aware of these non-dermatological symptoms of CVI, but the dermatological complications remain very unrecognized.
Cases and Methods
Six patients aging 33 to 84 years old with symptomatic chronic venous insufficiency (CVI) were referred to Alpha Vein Clinic in Las Vegas. Patients were found to also have overlain refractory LSC that were affecting their quality of life significantly, in average for the past 6 months. All the 6 had lesions compatible with CEAP classification C4 a/b and there were no ulceration present.
Skin biopsy was done in three that was compatible with LSC. Pathology showed hyperkeratosis, acanthosis, spongiosis, and patches of parakeratosis in the epidermis. All layers of the epidermis were thickened and there was elongation of rete ridges with pseudo-epithelium hyperplasia. patch test was performed in 2 that was negative. Fungal cultures were not done since the lesions did not resemble fungal infections as confirmed by dermatology.
These patients were followed and treated with either Radio Frequency ablation (RFA) (using Venefit Catheter), or Clarivein ablation (Mechanochemical endovenous ablation or MOCA) to treat their CVI, depending on the insurance preference (Figures 1,2).
Venefit™ targeted endovenous therapy is the only minimally invasive procedure to use segmental radiofrequency (RF) energy to provide an even and uniform heat to contract the collagen in the vein walls, causing them to collapse and seal the vein closed. After each segment is treated, the catheter is re-positioned to the next segment, and the process is repeated.
Mechanochemical endovenous ablation (MOCA), using the ClariVein® device (Vascular Insights, Madison, CT, United States), uses a rotating wire in a catheter to create mechanical damage to the endothelium of the vessel. At the same time, a sclerosant is infused at the end of the catheter.
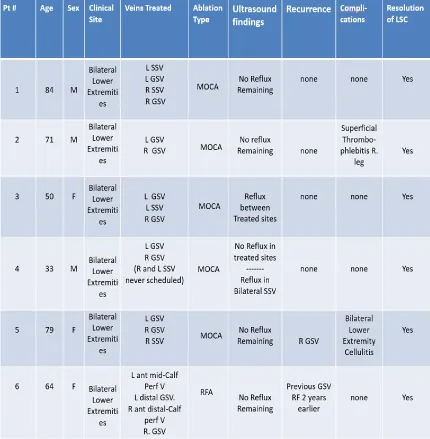
Venous ultrasound was used to look for residual reflux, deep venous thrombosis (DVT), or other potential complications at 3 days, 1 month, and 6 months. Patients were compared using descriptive analysis; looking at age, sex, clinical site, veins treated, ablation type, ultrasound findings, recurrence, clinical resolution of LSC and CVI as well as complications.
Findings and results are summerized in table 1.
Discussion
In our Clinic, we have observed a very strong correlation between LSC and underlying CVI. In fact, we have seen the following typical progression: CVI, local itch, local lesion, general pruritus, generalized LSC lesions, venous ulcer and super infections (especially of legs, arms and hands). The reflux of the perforator veins above the medial aspects of the ankles are of special importance because they are quite often the primary cause of the venous ulcers. The surrounding edematous, indurated and friable skin is vulnerable to cellulites which can further complicate the LSC lesions.
While the pathophysiology of LSC is attributed to a secondary reaction from the itch-scratch cycle and the subsequent local inflammatory reaction, the primary etiology has not been clearly elucidated in the literature [1, 2]. Some authors currently claim a relationship between underlying psychiatric pathology and a predilection to compulsively scratch as seen in cross-sectional [3], retrospective cohort [4], and case-control [5] studies. Recent studies postulate a correlation between LSC and peripheral neuropathy [4,6]. Increased frequency of degenerative spine conditions on MRI and radiculopathy on electrophysiological studies were observed in LSC patients compared to public. Case reports exist for instigation of LSC from herpes zoster [7], atopic dermatitis from hair dye [8], and nocturnal scratching [9]. A review of PubMed yielded zero results for LSC correlation with chronic venous insufficiency.
Chronic venous insufficiency most commonly presents with pruritus, with additional findings of leg heaviness and tightness according to the Bonn Vein study of 2,624 subjects [10]. Pruritus was not associated with age, gender, body mass index or region of living, with 95% confidence interval crossing one for all subsets. Stasis dermatitis which is a similar clinical entity has demonstrable correlation with venous insufficiency [11] as well. Recent histologic studies indicate utility of Gomori iron studies to differentiate stasis dermatitis from LSC, in addition to other common dermatoses, based on degree of iron staining [12].
Treatment for LSC remains controversial. Topical glucocorticoids remain a common initial treatment to reduce scratching [13]. Double-blind, multicenter, head-to-head trials of topical corticosteroids have been pursued in small study samples, with higher treatment success and quicker healing rates of halobetasol propionate ointment compared to diflucortolone valerate [14]. Case reports of treatment with gabapentin, topical tacrolimus, alitretinoin, and UVB exist and require confirmation but overall this has been an extremely hard to treat disease.
Our focus in vein clinic has been to address the CVI but somewhat accidently we noted the therapeutic effect on LSC. This was repeated in another 5 cases, as described. In one case, both upper and lower extremity severe pruritus and LSC resolved after lower extremity venous ablation. This can probably be a causal relationship explained by resolving circulating histamines in the entire body while treating the local CVI. All the cases were CEAP classification C4 a/b with no ulceration present and there might be a possibility that this category specifically brings the patients in (less symptoms with lower categories) and that our treatments overlap with it.
This incidental finding could provide a modality of therapy for a traditionally hard to treat entity with excellent success rate.
Conclusion
With the likely attribution of disseminated LSC lesions to local inflammatory mediators from CVI, we suggest an evaluation for venous vascular insufficiency for curative endovascular venous ablation in all patients with LSC. Further prospective randomized trials are recommended to further evaluate this.
- Valdes-Rodriguez R1, Stull C, Yosipovitch G (2015) Chronic pruritus in the elderly: pathophysiology, diagnosis, and management. Drugs Aging 32: 201-215. Link: https://tinyurl.com/ycrda3m4
- Yosipovitch G, Bernhard J (2013) clinical practice. Chronic Pruritus. New England Journal of Medicine 368:1625-1634. Link: https://tinyurl.com/y7cnkb99
- Kobuk N, Koca R, Atik L, Muhtar S, Atasoy N, et al. (2007) Psychopathology, depression and dissociative experiences in patients with lichen simplex chronicus. General Hospital Psychiatry 29: 232-235. Link: https://tinyurl.com/yb7adtf6
- Liao YH, Lin CC, Tsai PP, Shen WC, Sung FC, et al. (2014) Increased risk of lichen simplex chronicus in people with anxiety disorder: a nationwide population-based retrospective cohort study. British Journal of Dermatology 170: 890-894. Link: https://tinyurl.com/y8abmj7e
- Kouris A, Katoulis A, Christodoulou C, Rigopoulos D, Tsatovidou R, et al. (2015) Quality of life and obsessive-compulsive behavior in patients with lichen simplex chronicus. Journal of the German Society of Dermatology 13(2):162-163. Link: https://tinyurl.com/y92nqxjc
- Solak O, Kulac M, Yaman M, Karaca S, Toktas H, et al. (2009) Lichen simplex chronicus as a symptom of neuropathy. Clinical and Experimental Dermatology 34: 476-480. Link: https://tinyurl.com/yacekk96
- Gerritsen MJ, Gruintjes FW, Andreissen MA, van der Valk PG, van de Kerkhof PC (1998) Lichen simplex chronicus as a complication of herpes zoster. British Journal of Dermatology 138:921-922. Link: https://tinyurl.com/yajhurd7
- Chey WY, Kim KL, Yoo TY, Lee AY (2004) Allergic contact dermatitis from hair dye and development of lichen simplex chronicus. Contact Dermatitis 51: 5-8. Link: https://tinyurl.com/yawcklaz
- Koca R, Altin R, Konuk N, Altinyazar HC, Kart L (2006) Sleep disturbance in patients with lichen simplex chronicus and its relationship to nocturnal scratching: A case control study. Southern Medical Journal 99: 482-5. Link: https://tinyurl.com/y9vdy4dk
- Wrona M, Jöckel KH, Pannier F, Bock E, Hoffmann B, et al. (2015) Association of venous disorders with leg symptoms: results from the Bonn Vein Study. European Journal of Vascular and Endovascular Surgery 50: 360-367. Link: https://tinyurl.com/y9nhvulo
- Sippel K, Mayer D, Ballmer B, Dragieva G, Läuchli S, et al. (2011) Evidence that venous hypertension causes stasis dermatitis. Phlebology 26: 361-365. Link: https://tinyurl.com/yc22j8qm
- Northcutt AD, Tschen JA (2015) The routine use of iron stain for biopsies of dermatoses of the legs. Journal of Cutaneous Pathology 42: 717-721. Link: https://tinyurl.com/y755t562
- Lichon V, Khachemoune A (2007) Lichen simplex chronicus. Dermatology Nursing 19: 276. Link: https://tinyurl.com/y9upphuj
- Brunner N, Yawalkar S (1991) A double-blind, multicenter, parallel-group trial with 0.05% halobetasol propionate ointment versus 0.1% diflucortolone valerate ointment in patients with severe, chronic atopic dermatitis or lichen simplex chronicus. Journal of American Academy of Dermatology 25: 1160-1163. Link: https://tinyurl.com/y7onw4mb
Article Alerts
Subscribe to our articles alerts and stay tuned.
 This work is licensed under a Creative Commons Attribution 4.0 International License.
This work is licensed under a Creative Commons Attribution 4.0 International License.



 Save to Mendeley
Save to Mendeley
