International Journal of Vascular Surgery and Medicine
Right Iliofemoral Venous Thrombosis in a Prothrombin 20210GA carrier with Duplicated Inferior Vena Cava. An Unusual Case Report
Konstantinos Tigkiropoulos1*, Emmanouil Papadakis2, Ioannis Lazaridis1 and Nikolaos Saratzis1
2Hematology Department, Papageorgiou General Hospital, Thessaloniki, Greece
Cite this as
Tigkiropoulos K, Papadakis E, Lazaridis I, Saratzis N (2017) Right Iliofemoral Venous Thrombosis in a Prothrombin 20210GA carrier with Duplicated Inferior Vena Cava. An Unusual Case Report. Int J Vasc Surg Med 3(3): 043-045. DOI: 10.17352/2455-5452.000028Venous thromboembolism, presenting as deep vein thrombosis (DVT) is a disease affected by aging, with a low rate of about 1 per 10,000 annually before the fourth decade of life, rising rapidly after age 45 years, and approaching 5–6 per 1000 annually by age 80. We present the case of a 69-years old woman who presented to our emergency department with unilateral lower limb pain and swelling. Subsequent imaging revealed a right iliofemoral deep vein thrombosis, with associated duplication of her inferior vena cava. Thrombophilic screening revealed a prothrombin 20210A gene mutation. She was treated conservatively with Low Molecular Weight Heparin (LMWH) and elastic stockings.
Case Report
A 69-years old woman presented to the emergency ward with a 24 hour history of right leg pain with associated swelling. She was under treatment for osteoporosis and arterial hypertension. Her obstetrics history was free of pregnancy or miscarriage. On examination the right limb appeared swollen, warm with tenderness of calf muscles during palpation. Homans sign was positive. Sensation and motor function were not disturbed. Pulses were palpable in both legs. She didn’t report difficulty in breathing, tachycardia or pain in the chest. A provisional diagnosis of DVT was made and the patient was hospitalized for further investigation and treatment.
Investigations
Laboratory tests-Haematological (Hct:39 and INR:1,07) and biochemical- were normal on admission apart from D-Dimers which were markedly elevated (6.700 ng/ml-n.v<500). ECG showed sinus rhythm. Tumors markers (CEA, CA 15-3,CA 19-9, CA 125) were normal. Thrombophilia screen including Protein C, Protein S, Antithrombin III, APC Resistance-V, Factor VIII, homocysteine and Anticardiolipin antibodies was negative. A genetic thrombophilia test showed that patient is heterozygous for prothrombin G202101A gene.
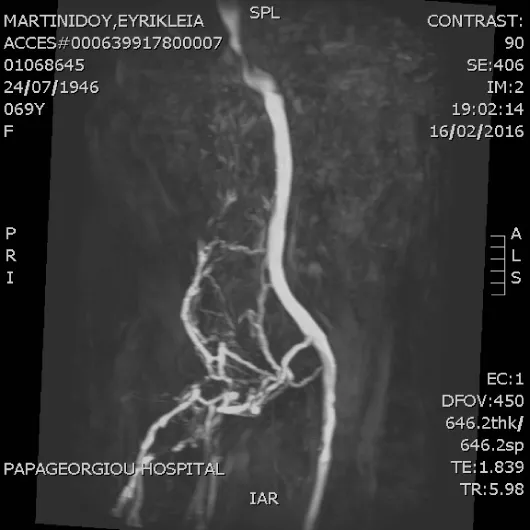
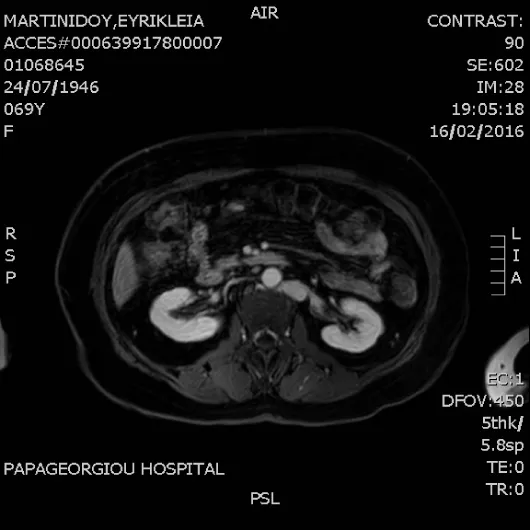
A U/S Duplex of the venous system was performed that confirmed thrombosis of the right common femoral extending to external iliac vein. A MR venography was scheduled to determine the extent of thrombosis. It revealed duplication of the inferior vena cava below renal veins with (Figures 1-3):
1. Thrombosis of the right IVC, common-external iliac veins, common femoral, superficial and deep femoral vein.
2. Venous drainage is performed via superficial collateral network from the left venous system.
3. Right internal iliac vein is drained through collateral venous network from the left internal iliac vein.
4. At the level of renal veins double IVC is joined retroaorticaly and cephalically it continues as azygos vein.
Treatment
In addition to the application of elastic stockings, patient was commenced on LMWH (Tinzaparin, 14000 anti-Xa IU,0.7 ml). Her anticoagulation therapy was initially planned to continue for 6 months in agreement with our Hemostasis specialist and to be reexamined in outpatient clinic after 3 months. She was discharged after 6 days in good clinical condition with oedema and pain been subsided.
Follow up
The patient was scheduled to perform an MRV 3 months after initiation of therapy with LMWH. It showed partial recanalization of the right inferior vena cava with increase of collateral circulation (Figure 4). The patient is followed up in outpatient department of hemostasis and vascular unit every 6 months and is under indefinite antithrombotic therapy with rivaroxaban 20mg.
Discussion
Venous thrombosis is a disease entity including deep vein thrombosis (DVT) and pulmonary embolism (PE), occurs with an incidence of approximately 1 per 1000 annually in adult populations [1]. It is a disease of aging, with a low rate of about 1 per 10,000 annually before the fourth decade of life, rising rapidly after age 45 years, and approaching 5–6 per 1000 annually by age 80 [2]. Etiology includes inherited and acquired factors. The most frequent site of venous thromboembolism (VTE) is deep vein thrombosis (DVT) of the legs [3].
Prothrombin G20210A gene mutation is the second most common cause of inherited DVT. It is present in 2 percent of the general population [4] and increases the risk of deep venous thrombosis by a factor of 2.7 to 3.8 [5,6].
Anatomical variations of the inferior vena cava occurs in 0.4‑4% of the population [7]. The most common variant is duplication of the inferior vena cava in 0.3-3% [8]. Which in most cases is identified incidentally. Double IVC is caused by persistence of left supracardinal veins during embryonic development, specifically between the sixth and tenth weeks of gestation [9]. It is believed that this venous malformation can predispose to DVT due to anatomical changes that promote venous stasis [10]. In our case, it was interesting that our patient was asymptomatic for a long time. She didn’t experience a miscarriage or pregnancy during reproductive period that could provoke venous thrombosis and her heterozygosity for prothrombin G20210A gene mutation could trigger the clotting cascade.
Anticoagulation therapy is the mainstay treatment of DVT. Warfarin, LMWH, direct oral anticoagulants and fondaparinux are the main modalities that can be used in inpatients as well as in outpatients. The duration of therapy depends on the triggering factor that causes thrombosis. Provoked thrombosis usually requires 3 months of therapy, whereas unprovoked thrombosis in the setting of inherited thrombophilia causes could need life-long treatment. Our patient may need indefinite anticoagulation therapy due to the presence of 2 risk factors, prothrombin G20210A mutation and double inferior vena cava with high risk of recurrency [11].
There are less than 20 cases series worldwide involving double IVC and venous thrombosis. Most of them concern young patients under the age of 35 years. It is not described any other case report worldwide associated with double IVC and thrombosis due to prothrombin gene G20210A mutation in a patient over 50 years old.
Consent
The patient has consented for the publication of case report.
- White RH (2003) The epidemiology of venous thromboembolism. Circulation 107: 14-18. Link: https://goo.gl/zW1Yug
- Silverstein MD1, Heit JA, Mohr DN, Petterson TM, O'Fallon WM, et al. (1998) Trends in the incidence of deep vein thrombosis and pulmonary embolism: a 25-year population-based study. Arch Intern Med 158: 585–593. Link: https://goo.gl/8upfiW
- Goldhaber SZ, Bounameaux H (2012) Pulmonary embolism and deep vein thrombosis. Lancet 379: 1835–1846. Link: https://goo.gl/JczRGS
- Rosendaal FR, Doggen CJM, Zivelin A, Arruda VR, Aiach M, et al. (1998) Geographic distribution of the 20210 G to A prothrombin variant. Thromb Haemost 79: 706-708. Link: https://goo.gl/osiHqK
- Poort SR, Rosendaal FR, Reitsma PH, Bertina RM, et al. (1996) A common genetic variation in the 3'-untranslated region of the prothrombin gene is associated with elevated plasma prothrombin levels and an increase in venous thrombosis. Blood 88: 3698-3703. Link: https://goo.gl/sZo2DQ
- Hillarp A, Zoller B, Svensson PJ, Dahlbäck B (1997) The 20210 A allele of the prothrombin gene is a common risk factor among Swedish outpatients with verified deep venous thrombosis. Thromb Haemost 78: 990-992. Link: https://goo.gl/VFQ8kU
- Mayo J, Gray R, Louis ES, Grosman H, McLoughlin M, et al. (1983) Anomalies of inferior vena cava. American Journal of Roentgenology 140: 339-345. Link: https://goo.gl/kNvVsg
- Bass JE, Redwine MD, Kramer LA, Huynh PT, Harris JH Jr (2000) Spectrum of congenital anomalies of the inferior vena cava: Cross-sectional imaging findings. Radiographics 20: 639–652. Link: https://goo.gl/RtAvjv
- Chuang VP, Mena CE, Hoskins PA (1974) Congenital anomalies of the inferior vena cava. Review of embryogenesis and presentation of a simplified classification. Br J Radiol 47: 206-213. Link: https://goo.gl/5Wq319
- Obernosterer A, Aschauer M, Schnedl W, Lipp RW (2002) Anomalies of the inferior vena cava in patients with iliac venous thrombosis. Ann Intern Med 136: 37-41. Link: https://goo.gl/RKsENf
- Marchiori A, Mosena L, Prins MH, Prandoni P (2007) The risk of recurrent venous thromboembolism among heterozygous of factor V Leiden or Prothrombin G20210A mutation.A systematic review of prospective studies. Haematologica 92: 1107-1114. Link: https://goo.gl/1EM1Y3
Article Alerts
Subscribe to our articles alerts and stay tuned.
 This work is licensed under a Creative Commons Attribution 4.0 International License.
This work is licensed under a Creative Commons Attribution 4.0 International License.



 Save to Mendeley
Save to Mendeley
