International Journal of Dermatology and Clinical Research
Expression profile of immunological and vascular mediators in an unusual case of paravertebral primary cutaneous non-Hodgkin lymphoma
Jeane Sousa Ribeiro1, Uener Ribeiro dos Santos2, Izaltina Silva-Jardim2, Jane Lima dos Santos2 and Juneo Freitas Silva3*
2Laboratory of Immunobiology, Department of Biological Sciences, Santa Cruz State University, Ilhéus-Itabuna Highway 16, Ilhéus, BA 45662-000, Brazil
3Center for Electronic Microscopy, Department of Biological Sciences, State University of Santa Cruz, Rodovia Ilhéus-Itabuna km 16, Ilhéus, BA 45662-000, Brazil
Cite this as
Ribeiro JS, Dos Santos UR, Jardim IS, Dos Santos JL, Silva JF (2020) Expression profile of immunological and vascular mediators in an unusual case of paravertebral primary cutaneous non-Hodgkin lymphoma. Int J Dermatol Clin Res 6(1): 019-021. DOI: 10.17352/2455-8605.000039Primary cutaneous follicle center lymphoma (PCFCL) is a rare type of indolent, low-grade cutaneous B-cell lymphoma, most frequent in trunk, particularly the head and scalp. Differential diagnosis for exclude other pathologies is needed. Here, we describers a detailed analysis on the expression profile of immunological and vascular mediators in tumor microenvironment that contribute to the knowledge, prognostic and diagnostic aid in a rare case of paravertebral PCFCL mimicking clinical appearance and localization of an unusual sebaceous cyst in a 48-year-old woman without history of neoplasia.
Introduction
The Primary Cutaneous Follicle Center Lymphoma (PCFCL), a subtype of primary Cutaneous Non-Hodgkin Lymphoma (CNHL), comprise 11-18% of all primary cutaneous lymphoma, most frequent in trunk, particularly the head and scalp, and the microenvironment are formed by a population of centrocytes and centroblasts [1,2]. The most studies referred the immunohistochemistry markers for this cells and other important markers. In some cases, a differential diagnosis is needed for acne cysts, epidermal inclusion cysts, arthropod bites and others [3]. The lesion can also appear in a rare location site and difficult diagnosis and treatment. Nevertheless, a more detailed analysis on the expression profile of immunological and vascular mediators in this type of lymphoma has not yet been performed but could contribute to the knowledge, prognostic and diagnostic aid [4]. The present report describes the expression profile of immunological and vascular mediators in an unusual case of paravertebral PCFCL at level of T4 in a 48-year-old woman.
Case report
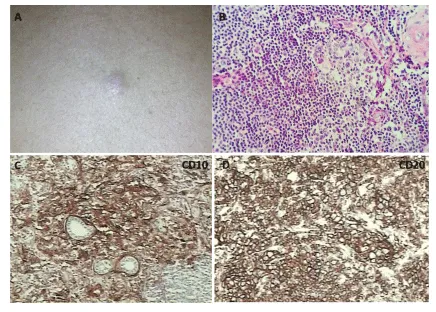
A 48-years-old previously healthy Brazilian woman with skin type IV according to Fitzpatrick’s classification, and without family history of neoplasia but with drug-controlled hypertension personal antecedent. She was referred to a dermatologist concerning the presence, for three months, of an “insect bite-like lump” on the back, associated with itching. She denied other symptoms. At the physical examination it was observed the presence of a well-defined, hard, solitary, pinkish nodular lesion, measuring 1.0 cm x 1.5 cm, adhered to the deep planes located in the left paravertebral region at the level of T4 (Figure 1A). Dermatologist suggested the diagnosis of appendage tumour (or appendix) or sebaceous cyst and the patient was referred for surgical removal of the lesion and subsequent histological analysis.
The skin biopsy revealed multifocal areas presenting nodular aggregates of small lymphocytes associated to medium to large lymphoid neoplastic cells in the dermis organized predominantly around blood vessels and apocrine glands, with fragmentation and loss of collagen fibers. These lymphoid cells had scanted to moderate amounts of pale eosinophilic cytoplasm and high nucleus-cytoplasm ratio, cleaved and elongated (large cleaved cells) or round or oval (centroblasts) nuclei, moderately coarse to fine chromatin and some cells had absent to inconspicuous nucleoli and others 1 to 2 distinct nucleoli. 0-3 typical mitoses and 0-1 atypical mitosis per field were observed in the 40X objective (Figure 1B). Occasional bi-nucleated cells were also observed.
The immunohistochemical study was carried out for Ki-67, CD10, CD20, BCL6, all with positive results. Negative reaction was identified for CD23, CD3 and anti-apoptotic protein Bcl-2. The ki-67 index was approximately 80% (Table 1).
Based on the histopathologic and immunohistochemical findings, the diagnosis was a primary cutaneous follicle center lymphoma (PCFCL), with the expression of CD20+ and CD10+ (Figure 1C,D). The negativity of BCL2 possible favoured primary involvement of the skin.
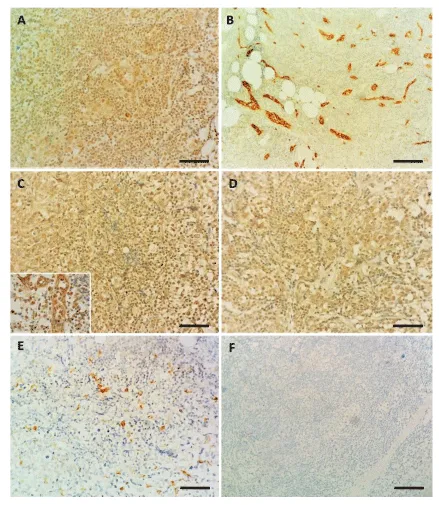
VEGF strong expression was observed not only in the vascular endothelium as well as in all lymphoid cells of the tumor microenvironment (Figure 2A). The neoplasm was well vascularized with the blood vessels exhibiting the cuboidal and reactive endothelium evidenced by FVIII expression (Figure 2B). The immunohistochemical analysis of INF-γ and MIF revealed strong nuclear and/or cytoplasmic expression in the lymphoid population of the tumour, with strong expression in blood vessels, while iNOS immunoexpression was cytoplasmic, discrete to moderate in some cells, mainly in centroblasts and large cleaved cells (Figure 2C-E).
After the removal of the lesion, histological analysis and immunohistochemical study, the oncologist requested a PET-CT scan. With no other organ involved after thorough investigation for staging purposes, the patient was underwent 25 series of local radiation treatment, and has been under follow-up care.
Quarterly review was indicated. Laboratory tests Cholesterol (LDL), total cholesterol, creatinine, lactic dehydrogenase, alkaline phosphatase, fasting glycemia, aminotransferase aspartate, alanine aminotransferase, platelet counts, T3, T4 and TSH tests, Beta-2-Microglobulin are within normal limits in all reviews. Imaging tests (upper and lower abdomen ultrasound and chest X-ray) remain unchanged. The patient evolved without relapses until the moment, 04 years after diagnosis.
Discussion
Non-Hodgkin’s lymphomas (NHL) represent 90% of all lymphomas and around 85-90% of this are B-cells lymphomas [5]. The PCFCL is an indolent lymphoma that present commonly solitary plaques, typically occurs in middle aged to older people, most predominant in male, in 50% of cases involve head and neck regions, and multifocal skin lesions are rare [6]. A study in Brazil showed that PCFCL represent only 10.2% of all cases for primary cutaneous lymphoma with a good 5-year cumulative survival rate [7].
Some cases need a differential diagnosis because of cutaneous neoplasia’s and inflammatory lesions that mimicking the cutaneous lesions of PCFCL [3]. Although the trunk be a frequent site, PCFCL with cutaneous locations in paravertebral region is less common and at the level of T4 is rare in literature. This location is more frequently associated with other types of NHL, with skeletal muscle [8] and spine [9], involvement, usually associated with pain. But in this case PET-CT reveled no other organ involved and no pain episode was related by the patient.
The negativity of BCL2 probable favoured primary involvement of the skin and the high expression of FVIII and VEGF demonstrates the high vascularization of lymphoma. A previous study showed a high intratumorally expression levels of VEGF and microvascular density in primary cutaneous B-cell lymphomas, with PCFCL presenting an intermediate vascular density when compared with more aggressive types4. The strong expression of VEGF was observed not only in the vascular endothelium as well as in all lymphoid cells of the tumor microenvironment.
The positivity of MIF also contributes to angiogenesis and growth of lymphoma [10]. Besides that, the strong nuclear and/or cytoplasmic expression for INF-γ can indicate an inflammatory microenvironment that positively contribute to this good prognose of patient. Together the findings confirmed the diagnosis of PCFCL and the expression profile of immunological and vascular mediators can be successful to clarify the tumor microenvironment and prognosis.
- Klemke C (2014) Cutaneous lymphomas. J Ger Soc Dermatology 12: 7-30. Link: https://bit.ly/37hXS0O
- Selva R, Violetti SA, Delfino C, Grandi V, Cicchelli S, et al. (2017) A Literature Revision in Primary Cutaneous B-cell Lymphoma. Indian J Dermatol 62:146–157. Link: https://bit.ly/2HfDNNz
- Suárez AL, Pulitzer M, Horwitz S, Moskowitz A, Querfeld C, et al. (2013) Primary cutaneous B-cell lymphomas: Part I. Clinical features, diagnosis, and classification. J Am Acad Dermatol 69: 329.e1-329.e13. Link: https://bit.ly/37baFCl
- Wobser M, Siedel C, Kneitz H, Bröcker EB, Goebeler M, et al. (2013) Microvessel density and expression of vascular endothelial growth factor and its receptors in different subtypes of primary cutaneous B-cell lymphoma. Acta Derm Venereol 93: 656–662. Link: https://bit.ly/2Iuf4Wv
- Ekström-Smedby K (2006) Epidemiology and etiology of non-Hodgkin lymphoma - A review. Acta Oncol (Madr) 45: 258–271. Link: https://bit.ly/2H7eEVN
- Wilcox RA (2018) Cutaneous B-cell lymphomas: 2019 update on diagnosis, risk stratification, and management. Am J Hematol 93: 1427-1430. Link: https://bit.ly/2HalSbd
- Nudelmann LM, Bonamigo RR (2015) Primary cutaneous lymphoma in southern Brazil: A 12-year single-center experience. Int J Dermatol 54: e512–e520. Link: https://bit.ly/37bbmvr
- Diniz RE, Goldenberg J, de Carvalho JC, Gomes CE, Goldenberg ED, et al. (1995) Lymphoma of unknown origin located in paravertebral muscles: an unusual cause of low back pain in children. Sao Paulo Med J 113: 953–956. Link: https://bit.ly/345NEyD
- Moussalay E, Nazha B, Zaarour M, Atallah JP (2015) Primary non-hodgkin’s lymphoma of the spine: A case report and literature review. World J Oncol 6: 459-463. Link: https://bit.ly/3j0jD7G
- Talos F, Mena P, Fingerle-Rowson G, Moll U, Petrenko O (2005) MIF loss impairs Myc-induced lymphomagenesis. Cell Death Differ 12: 1319-1328. Link: https://bit.ly/37gGzxk
Article Alerts
Subscribe to our articles alerts and stay tuned.
 This work is licensed under a Creative Commons Attribution 4.0 International License.
This work is licensed under a Creative Commons Attribution 4.0 International License.

 Save to Mendeley
Save to Mendeley
