International Journal of Dermatology and Clinical Research
The extended modified male Z-plasty necklift for correction of severe aging changes of the neck with secondary improvement of the lower third of the face
Gary J Nishioka*
Cite this as
Nishioka GJ (2018) The extended modified male Z-plasty necklift for correction of severe aging changes of the neck with secondary improvement of the lower third of the face. Int J Dermatol Clin Res 4(1):008-010. DOI: 10.17352/2455-8605.000027The male Z-plasty necklift (MZPN) is a well described procedure [1-4], specifically used for men with severe aging neck changes who cannot be achieve a satisfactory aesthetic outcome with other necklift procedures that are performed through a submental incision. Other direct excision male necklift techniques have also been described [5-9]. The MZPN is not felt suitable for women because of the visible anterior neck incision which does not camouflage well with thinner smooth non-hair bearing neck skin, and an elective long visible scar located here is generally considered socially unacceptable. However, for men with severe aging changes of the neck this procedure produces results with a very high level of patient and surgeon satisfaction. Furthermore, surgical morbidity is very low with rapid recovery, and can easily be performed in the office surgery suite with local anesthesia with or without light sedation.
This manuscript describes an extended MZPN which also enhances the lower third of the face producing a facelift-like effect with no increase in surgical morbidity and no significant increase in visible scarring with the patient in the natural head position.
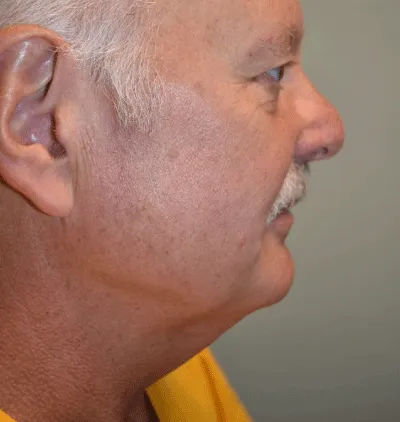
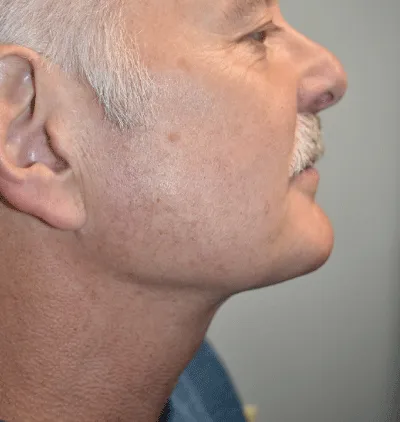
The design of the incision marking outline from a frontal submental view has a “gourd-like” shape with a horizontal stem on top representing the submental incision. Inferior extension of the excision generally extends to or into the supra-sternal notch. The isthmus of the gourd-like shape is made at the planned cervicomental angle where a single Z-plasty is placed. The boundary is marked using a pinch technique with marking just inside (1 cm) the finger-tip contact of the pinched skin soft tissue as general conversion factor based on experience (Figure 1). The island of skin is excised in the subcutaneous plane with de-fatting to the superficial surface of the platysma muscle (Figure 2). Undermining is performed laterally in the subcutaneous plane with a liposuction cannula with or without fat tissue removal. A submental platysmaplasty is performed with bilateral platysma muscle release incisions at the planned cervicomental angle with sub-platysmal fat removal as needed to permit an aesthetic submental contour upon closure (Figure 3). Generally, the platysma muscles do not require re-approximation and suturing caudad (inferior) to the planned cervicomental angle but horizontal release incisions of the plastysma at the suprasternal notch region may be needed to ensure the plastysma lays flat. Skin flap trimming and in-setting in the submental region is required to achieve a smooth contour. The Z-plasty and remainder of the soft tissue flap closure requires strategically placed deep dermal support sutures such as 4-0 or 3-0 Vicryl as there is significant tension (Figure 4). It is the tension with closure of the soft tissue flaps in the submental area that produces a significant tightening effect on the lower third of the face, producing a natural appearing facelift-like effect. Deep dermal sutures are placed in non-tension areas with 5-0 Vicryl followed by 5-0 fast resorbing gut for the skin surface closure (Figure 5). An immediate aesthetic benefit is seen from the profile view after completion of the procedure (Figure 6). The incision line can be taped with mastisol and steri-strips or left open. A light spandex support garment is placed for general comfort and protection of the surgical site as there is very little discomfort after 24 hours, and patients need a reminder that they just had surgery and need to be mindful about activity level. Because of the tension produced by the wound closure there is no potential space for hematoma formation. The spandex garment is used for one week and is removed for showering and for respite breaks as needed. The patient may shave over the incision line at one week but with an electric razor is recommended initially. No complications have been encountered in over 20 years. The most common sequelae that is encountered is development of a hypertrophic scar along some the part of the incision (less than 10% of patients), and these patients receive Kenalog injections (steroid) to these affected areas. A consistent surgical outcome seems universally achieved with a significant (dramatic) contour benefit of the neck as well as the lower third of the face (Figures 7-10*).
(The patients used in the figures have provided written consent for use of their photographs for “education and research purposes”, and are located in their respective electronic medical record system files.)
- Gradinger GP. (2000) Anterior cervicoplasty in the male patient. Plast Reconstr Surg 106: 1146-1154. Link: https://goo.gl/Eby6ae
- Thomas C, Biggs TM. (1971) The T-Z-plasty for the male “turkey gobbler” neck. Plast Reconstr Surg. 47: 534-538. Link: https://goo.gl/ZT356e
- Biggs TM, Steely RL. (2000) The male neck and T-Z-plasty: 28 years later. Aesthetic Surg J 1: 31-34. Link: https://goo.gl/qXJFCk
- Miller TA. (2005) Excision of the redundant neck tissue in men with platysma plication and Z-plasty closure. Plast Recontr Surg 115: 304-313. Link: https://goo.gl/QXTuRJ
- Parsa FD, Parsa NN, Castel N. (2016) A modified, direct neck lift technique: the cervical wave-plasty. Arch Plast Surg 4392: 181-188. Link: https://goo.gl/TdPzkb
- Chaput B, Grolleau JL, De Bonnecaze G, Eburdery H, Chavoin JP, et al. (2012) Anterior medial cervicoplasty. Ann Chir Plast Esthet 57: 612-617. Link: https://goo.gl/HSkkQU
- Bitner JB1, Friedman O, Farrior RT, Cook TA. (2012) Direct submentoplasty for neck rejuvenation. Arch Facial Plast surg. 9: 194-200. Link: https://goo.gl/AQdBik
- Bruneau S1, Nguyen P, Foletti JM, Bellot V, Casanova D, et al. (2013) Neck rejuvenation by anterior cervicoplasty: an original technical modification. J Plast Reconstr Aesthet Surg 66: 1627-1628. Link: https://goo.gl/m7wgN1
- Jordan JR, Yellin S. (2014) Direct cervicoplasty. Facial Plast Surg. 30: 451-461. Link: https://goo.gl/3r3fEp
Article Alerts
Subscribe to our articles alerts and stay tuned.
 This work is licensed under a Creative Commons Attribution 4.0 International License.
This work is licensed under a Creative Commons Attribution 4.0 International License.









 Save to Mendeley
Save to Mendeley
