International Journal of Dermatology and Clinical Research
A Comprehensive Survey on Models Used for Acnegenesi
Nituporna Bora1* and Jutirani Devi2
1PG scholar, NETES Institute of Pharmaceutical Science, Santipur, Mirza, Assam, India
2Assistant professor, NETES Institute of Pharmaceutical Science, Santipur, Mirza, Assam, India
Cite this as
Bora N, Devi J. A Comprehensive Survey on Models Used for Acnegenesi. Int J Dermatol Clin Res. 2024;10(1):005-012. Available from: 10.17352/2455-8605.000051Copyright
© 2024 Bora N, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.Acne vulgaris is a widespread chronic inflammatory skin illness that is primarily caused by inflammation, irregular skin cell turnover inside hair follicles, increased sebum production, and Propionibacterium acnes bacterial overgrowth. This comprehensive overview examines the intricate causes of acne vulgaris. The paper highlights the significant role of genetic predisposition, hormonal fluctuations, and environmental factors in acne development. Various in vivo and in vitro models, including mouse ear edema, rat models, and advanced techniques like 3D bioprinting and organ-on-a-chip systems, are discussed for their utility in studying acne pathogenesis and testing therapeutic interventions. The review underscores the importance of integrating diverse models to enhance understanding of acne mechanisms and improve treatment strategies, while also acknowledging the limitations of current models in replicating the complexity of human skin. Future research should focus on refining these models to better capture the multifactorial nature of acne and facilitate the development of effective, targeted therapies.
Introduction
The microorganism named Propionibacterium acnes (P. acnes) and the glands that produce oils are the main causes of acne vulgaris, a chronic inflammatory dermatological condition marked by inflamed regions, whiteheads, and blackheads. This dermatological condition is the ninth most prevalent illness in the entire world, affecting about 85% of people between the ages of 14 and 25. Some cases of this syndrome continue into adulthood. Acne is common, with epidemiological studies indicating that between 20% and 95% of people will get it at some point. Acne is a multifaceted inflammatory disease that is impacted by several variables. Four main mechanisms are primarily responsible for the formation of acne lesions: inflammation, altered follicular keratinization, increased sebum production, and P. acnes colonization of the pilosebaceous unit. Developing efficient therapies and management plans for this prevalent condition requires an understanding of these mechanisms [1,2]. Staphylococcus epidermidis and Propionibacterium acnes, as well as Pseudomonas aeruginosa, are two Gram-positive and Gram-negative bacteria that are the primary cause of acne [3,4]. Acne is also influenced by other variables, including hormones, food, and heredity. When androgen hormones are released throughout puberty, they cause the sebaceous glands to generate more oil, which clogs pores and causes acne and blackheads [2,5]. To control SG activity, a variety of sex hormones are needed, including corticotropin-releasing hormone, adrenocorticotropic hormone, estrogens, androgens, tyrosine kinase hormones, melanocortins, and glucosecoid [6,7]. In preclinical research, ear models implanted subcutaneously or intradermally in rabbits, rats, and mice are frequently used for pharmacodynamic screening associated with acne. The inflammatory response and bacterial Colony-Forming Units (CFU), which are important elements in the development of acne, can be evaluated by researchers using these models. These models are useful for studying the four main factors that contribute to acne pathology: inflammation, bacterial colonization, aberrant follicular keratinization, and hyperseborrhea. Researchers can assess possible treatments and gain a better understanding of acne causes by looking into these characteristics [8,9].
By the utilization of 3D printing technology, layers of bioink-which may include layers of tissues, growth factors, and other materials-are printed to produce live tissue frameworks, such as skin cells. 3D bioprinting is often used to generate individualized skin grafts or personalized skin models to assess novel acne treatment options.
Using biological cells of the skin and microfluidic channels, an organ-on-a-chip device mimics the environment of human cells on a microchip. This technique can assist in studying how topical treatments or acne drugs affect skin cells, enabling researchers to see how the skin reacts to different treatments without using human subjects. Both strategies facilitate personalized and successful acne treatments [10,11].
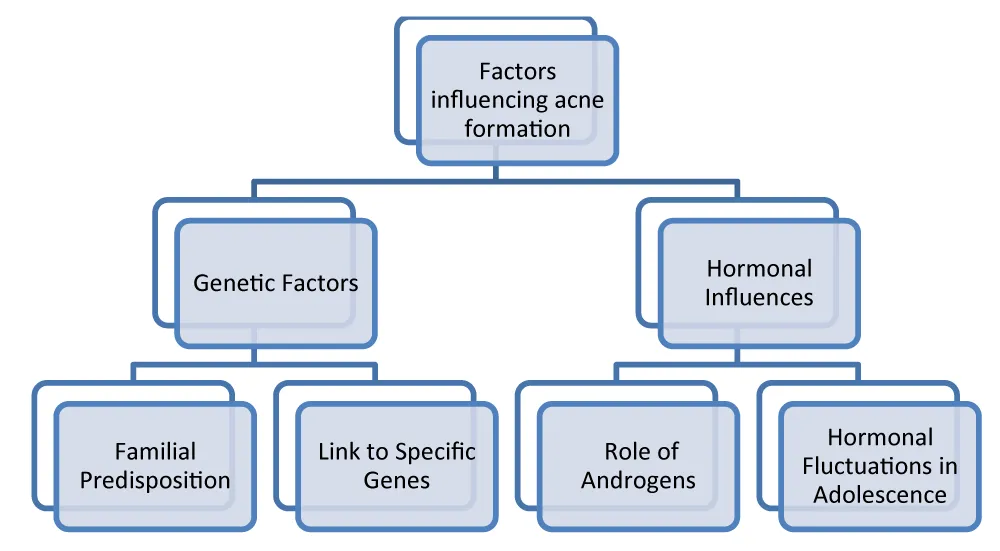
Factors responsible for acne [12-14] (Figure 1)
Pathogenesis of acne
1. Formation of comedones
- Sebum production: Propionibacterium acnes thrives in an environment that is facilitated by an abundance of sebum and an aberrant keratinization process. The pathophysiology of acne lesions is further complicated by these bacteria, which are essential to the inflammatory cascade. Sebum’s function goes beyond its amount. Changes in its makeup can affect the follicular plug’s consistency and accelerate the development of acne lesions [15-17].
- Role of hyperkeratinization: The initial step of the formation of visible comedones, microcomedones, is caused by hyperkeratinization, a process in which follicular epithelial cells exhibit aberrant proliferation and differentiation. Genetic factors may play a role in this complex event by increasing susceptibility to hyperkeratinization., which in turn may affect the pace of follicular cell shedding and ultimately result in the formation of comedones [18-20].
2. Inflammatory response
- Activation of immune cells: Immune cells including neutrophils and macrophages infiltrate the site of inflammation, causing redness and swelling in inflammatory acne lesions. Pro-inflammatory cytokines are released when bacteria activate Toll-Like Receptors (TLRs), prolonging the inflammatory response. Although the immune response aims to eradicate infections, it also worsens tissue damage and has a role in the clinical appearance of acne [21-23].
- Cytokine release and inflammation: Cytokines such as interleukins (IL) and the alpha form of tumor necrosis factor (TNF-a) are important in the inflammatory circumstances of acne. In reaction to bacterial components, the immune cells release IL-1b, which intensifies the inflammatory response. TNF-a facilitates the influx of immune cells and triggers the secretion of Matrix Metalloproteinases (MMPs), which ultimately results in tissue damage. Large acne formations develop as a result of the inflammatory process that carries on next to the acne scar and damages the surrounding tissue. The development of nodules and cysts, which are indicative of many forms of acne and may leave scars, can be caused by inflammation [24-26].
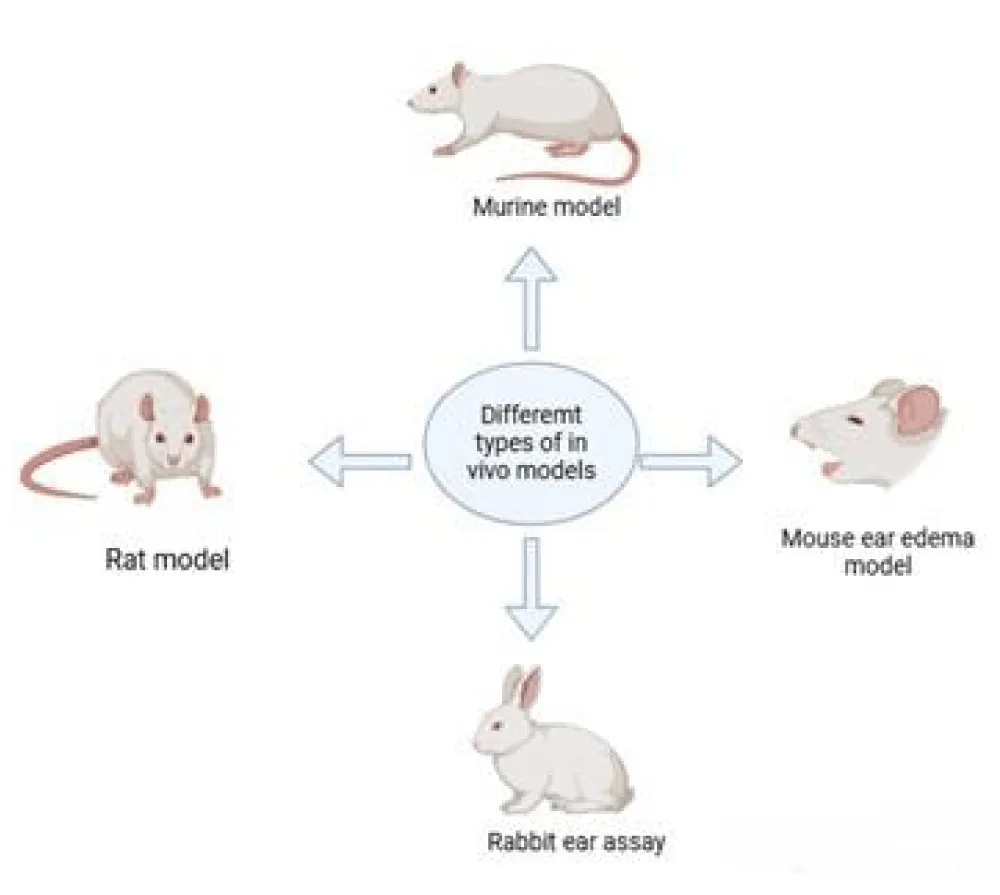
In vivo acne models (Figure 2)
1. Mouse-ear edema model
In this study, RDL’s impact on inflammation caused by P. acnes was evaluated using ICR mice. Each mouse received an intradermal injection of acne-causing bacteria (6 × 10^7 CFU in 20 μL Phosphate buffer saline) in its left ear. Twenty microliters of Phosphate buffer saline were injected into the identical mice’s right ear as a control. Following the bacterial injection, intradermal injections of RDL in different dosages (100, 300, and 1000 μg per 20 μL in PBS) were administered to the P. acnes-injected and PBS-injected sites. Additionally, an identical amount of phosphate buffer saline (20 μL) was injected into each ear as a control. The effects of RDL on inflammation in the presence of P. acnes were assessed using this experimental design in comparison to a control group that was not infected [27].
The animals were put unconscious after each treatment phase, and 24 hours after the injection, their ears were taken. On the day of sacrifice, the weight and thickness of each mouse’s ears were noted. By analyzing the weight of the left (injected with P. acnes) and right (injected with PBS) ear disks, the extent of edema was ascertained. The weight and thickness of the P. acnes-injected ear were also measured as a percentage of the PBS-injected control to gauge the inflammatory response. This method produced valuable data regarding the impact of RDL therapy on inflammation caused by P. acnes [28].
The ear was removed 24 hours following the P. acnes injection, and a sample was taken for bacterial quantification using a 6 mm biopsy punch. A hand tissue grinder was then used to homogenize the biopsies in 200 μL of sterile PBS. Serial dilutions of the homogenate (from 1:102 to 1:108) were plated onto RCM agar plates to count the P. acnes colony-forming units (CFUs) in the ear. To allow for colony formation, these plates were kept at 37 °C for 72 hours in an anaerobic environment. Following this, the colonies were counted. This method helped determine the efficacy of the therapies by providing a quantitative assessment of P. acnes in the ear tissue. [29].
- Benefits:
- Inflammation mimicry: It is useful for testing anti-inflammatory acne treatments since it accurately simulates acute inflammatory responses.
- Cost-effective: This model is reasonably priced because rats require less upkeep than larger animals.
- Well-established: With established protocols, it is a popular and well-understood model in dermatology research.
- Drawbacks:
- Limited acne relevance: The form and distribution of sebaceous glands in rat skin differ greatly from those in human skin, making it difficult to directly apply to studies on acne.
- Invasive: To create inflammation, the model frequently calls for skin irritation or drug injections, which can be intrusive and upsetting.
- Not always representative: It might not accurately reflect the pathophysiology of human acne, especially the contribution played by bacteria or sebum production.
2. Rat model
It is possible to successfully create acne on a rat model by continuously applying an oleic acid smear. Rats’ dorsal skin exhibits thickening and hardening of local tissue, as well as red papules that are created by hair follicle ridges, all of which are examples of animal model performance replication. Subjectively, after dermal application of the drug, the rat skin’s roughness and amount of acne use decreased significantly. However, the distinctions between the six categories need to be shown more subjectively and intuitively, for example, via data and graphics. Thus, immunohistochemical pathology and HE staining were employed to observe.
In this investigation, Sprague Dawley rats of both genders of SPF grade, with an average weight of 180 g – 220 g, were used. The experimental circumstances, which included temperatures of 20 ± 2 °C, 60 ± 5% humidity, and a cycle of twelve hours of light and darkness, were given to the rats for a week to allow them to get used to them. To reduce the animals’ pain and suffering during the trial, all procedures were carried out under anesthesia using 10% chloral hydrate. The goal of the meticulous anesthetic and condition management was to give the experiments a controlled and compassionate setting [28].
In another study, mature male Sprague Dawley rats (SD rats) weighing 220 ± 20 g were given an acne model made with 80% oleic acid. In controlled conditions, the rats were housed in conditions with a cycle of twelve hours of light and darkness, temperatures between 19 and 23 °C, and moisture levels around 40 and 65%. Blinding was maintained throughout the testing and analysis of data phases, and the rats were split up into groups for experimentation using a randomly assigned block design.
The rats were randomly allocated to either the model group or the control group. The acne model was created by applying 2.0 mL of eighty percent oleic acid daily for 14 days to a 4 cm bald spot on the rats’ backs. Following the establishment of the acne model, the rats were further divided into the medication distribution group and the acne model group using a random number control table. Animals in the medicine group received each week a dose of 1.0 g of medication, while animals in the Control group and Model groups received no medication at all. This study aimed to evaluate the impact of the medicine on acne lesions caused by oleic acid [30,31].
- Benefits:
- Sebum simulation: Since oleic acid is a crucial part of sebum, this model triggers a sebaceous reaction, which makes it applicable for evaluating acne-related medications.
- Inflammation induction: It causes inflammation, which is essential to the pathophysiology of acne, and makes it possible to assess anti-inflammatory medications.
- Ease of induction: Oleic acid can be used topically or systemically to induce the model, making it easy to use for large-scale research.
- Drawbacks:
- Inconsistent acne formation: The model is not entirely dependable for researching acne since not all rats exposed to oleic acid develop obvious lesions resembling acne.
- Minimal human significance: Results may not be directly applicable to treating acne in humans since rat skin and glands that produce oil differ from those of humans.
- Involves no bacterial factors: Inflammation brought on by oleic acid ignores the bacterial component of acne, which is critical in human acne.
3. Murine model of acne
In this investigation, six male mouse strains BALB/c weighing around nineteenth and twenty-one g at 8 weeks of age were employed. Each mouse was housed in a separate cage that featured a 12-hour light/dark process, 22 ± 2 °C, and 50 ± 10% relative humidity. The mice were randomly assigned to either the P. bacterium. acnes + Synthetic Sebum Group (PA) or the No Treatment Group (NT). They can eat and drink everything they want.
Approximately 5 × 10^8 colony-forming units per ml of acne-causing bacteria in 50 μL of BHI medium was injected intradermally into the mice on the day after they were shaved beforehand. Following the injection, the skin was treated with 20 μL of newly made synthetic sebum, which contained 13% squalene, 45% triolein, 25% jojoba oil, and 17% oleic acid. For three days, this application was made every day.
Every day, optical image detection was carried out to track the development of lesions, and lesions were aseptically removed for analysis at prearranged intervals. Anaerobic incubation was used to measure the colony-forming units (CFUs) on agar plates. The main reason for this study was to see how P. acnes and synthetic sebum affected the formation of acne lesions in a mouse model [32].
- Benefits:
- Genetic similarity: Mice and humans have a lot in common genetically, which is advantageous when researching the genes and mechanisms underlying acne.
- Controlled studies: By precisely controlling genetic background, environmental factors, and treatment interventions, murine models improve experiment reproducibility.
- Inclusion of multiple causes: Mice models can be modified to investigate bacterial causes, inflammation, and sebaceous gland activity, among other features of acne.
- Drawbacks:
- Skin structure differences: Because mouse skin differs from human skin in terms of its glands that produce oils and hair follicles, it cannot be directly applied to acne treatments.
- Limited relevance to human acne pathology: Mice generally require induction to develop acne, which may not accurately mimic human acne.
- Ethical concerns: As with all animal testing, there are ethical considerations regarding the use of mice, particularly concerning the distress caused by the induction of acne.
4. Rabbit ear assay
Indeed, a popular model for assessing a compound’s comedogenicity is the rabbit ear assay (REA). It works well as a screening tool for both topical and follicular skin irritants, as you indicated. The REA’s sensitivity is one of its benefits; it can identify negative skin reactions including erythema, desquamation, and follicular keratosis quickly—typically within two weeks of daily use. This rapid assessment is particularly useful because many commercial products can take several months to produce similar effects on human skin. Furthermore, findings from the REA tend to correspond well with human outcomes, making it a trustworthy indicator of possible comedogenicity in cosmetic and pharmaceutical formulations. This model helps researchers and formulators better understand the risks associated with different ingredients, leading to safer products for consumers [33].
Although the rabbit ear assay is a helpful tool for determining comedogenicity, it draws attention to important distinctions between animal and human skin that may affect how results are interpreted. One notable difference is that bacteria like Propionibacterium acnes, which are essential to the inflammatory processes linked to human acne vulgaris, do not colonize the REA. Furthermore, because there is no follicular wall breach, the REA does not develop inflammatory lesions, and its keratin structure is different, with the horn being less densely packed. Moreover, rabbits are easier than humans to mechanically expel comedones. These variations highlight the need for additional human studies to ensure safety and efficacy, indicating that although the REA can successfully screen for comedogenicity, its results should be interpreted cautiously as they might not accurately predict human skin reactions [34,35].
- Benefits:
- Large ear surface: Rabbits’ ears are comparatively large and accessible, which makes them useful for applying topical treatments and evaluating the effects of medications.
- Closer to human skin: Compared to rats, rabbits’ skin is more relevant to studies on acne since it resembles human skin in structure and contains sebaceous glands.
- Visible lesions: Effectively inducing acne-like lesions enables a visible evaluation of the effectiveness of treatment.
- Drawbacks:
- Cost and size: Compared to rodents, rabbits require greater upkeep, which could raise the price of extensive research.
- Limited reproducibility: Results from different tests may differ due to variations in rabbit skin and acne production.
- Ethical issues: Using rabbits in these kinds of experiments has ethical issues, particularly when it comes to the model’s invasiveness when it comes to causing and treating acne lesions.
In vitro models for acne
1. Follicle model
P. acnes, keratinocytes, and sebocytes are evaluated about one another using the follicular model. P. acnes colonize PSU and superficial skin. To better understand how sebocytes and keratinocytes interact with Propionibacterium acnes, A permeable polyester membrane divided the two chambers in which the investigators co-cultured conserved sebocytes (SZ95) and keratin cells (HPV-KER). This allows ehaviour molecules to be exchanged while maintaining distinct cellular environments, and by studying this co-culture model, researchers hope to clarify how sebocytes affect keratinocyte ehaviour and vice versa, especially in the context of P. acnes colonization and its role in acne development. This allows for the examination of lipid production, inflammatory responses, and microbial interactions, which can provide insights into the pathophysiology of acne and possible treatment targets. Soluble molecules don’t spread throughout the chambers thanks to the porous polyester membrane. P. acnes is restricted to the hair follicular cells in the healthy PSU [36,37].
2. Testosterone-Induced Acne Model (TIAM)
One steroidal hormone that causes various types of acne is testosterone. Through its follicular receptor, keratin is stimulated by the conversion of testosterone to dihydrotestosterone [38]. Because of the increased size and activity of SG, acne is caused by both testosterone and dihydrotestosterone. When assessing the effectiveness and biocompatibility of the various components, the TIAM is a valuable tool [39].
3. SG organ culture
By removing human skin (from cadavers, donors, and other sources) or by microdissection and shearing, these models are created in isolation from SG. Eagle’s medium is changed with Dulbecco and the isolated specimens are promptly placed in it. Following the isolation of the specimen, the remaining dermal sections are immediately inserted into the growth medium once the epidermal layers have been separated. To test the lipogenesis rate in acne-affected people and the impact of substrates on lipid rates, Dermal and epidermal components are either present or absent in intact SGs. It was possible to cultivate SG-derived cells by seeding the separated SGs over a 3T3-cell feeder level and complete culture media in Petri plates. It involved incubating the cultures. The basal and differentiated cell layers can have their proliferation and lipid production investigated concurrently [40].
For anti-acne research employing animal-isolated SG culture, the SG in situ model is appropriate. To calculate the effects of nerve growth factor, substance P, neuropeptide Y, vasoactive polypeptide which are found in the intestine, and calcitonin gene-related peptide, Toyoda and Morohashi conducted organ culture on SG obtained from mice. By increasing the rate of differentiation and proliferation, substance P treatment of SG caused the control glands to produce fewer lipids, suggesting that stress and acne cause acne and acne scarring [41].
4. 3D bioprinting in acnegenesis models
3D bioprinting involves layering living cells, biomaterials, and growth factors to construct skin models that closely resemble natural tissue. These models can include various skin components, such as sebocytes (sebaceous gland cells), keratinocytes (epidermal cells), and immune cells, allowing for a comprehensive study of acne development [42,43].
5. Applications in acne research
Skin microenvironment: 3D bioprinted skin models can replicate the architecture of human skin, including hair follicles and sebaceous glands, providing an ideal environment to study the factors involved in acne formation, such as irritation, colonization of bacteria, and elevated oil production.
Testing therapeutics: These models can be used to check the effectiveness of topical and systemic acne treatments, allowing researchers to assess how well these therapies penetrate the skin and their effects on acne-related pathways.
Studying disease mechanisms: Researchers can manipulate various components within 3D bioprinted models to simulate acne triggers, such as hormonal changes or microbial infections, enabling a deeper understanding of the molecular mechanisms that lead to acne development.
Personalized medicine: 3D bioprinting offers the creation of patient-oriented skin models using cells derived from individuals with acne. This customization helps researchers evaluate how different patients may respond to treatments based on their unique skin biology.
6. Organ-on-a-chip systems in acnegenesis models
Organ-on-a-chip (OOC) systems are microfluidic devices that integrate living cells in a way that mimics organ functions. For acne research, these systems can replicate the conditions of human skin and its sebaceous glands [44,45].
7. Applications in acne research (Table 1)
Dynamic study of sebaceous glands: OOC systems can simulate the function of sebaceous glands, allowing researchers to investigate how various factors, such as hormones (e.g., androgens) and bacteria (e.g., Propionibacterium acnes), influence sebum production and contribute to acne formation. Inflammation Modeling: By incorporating immune cells and inflammatory mediators into the OOC system, researchers can study the inflammatory response associated with acne, providing insights into how inflammation exacerbates the condition.
Response testing: OOC systems allow for real-time monitoring of drug interactions with skin cells. Researchers can test the efficacy of acne treatments and observe their impact on cellular behavior, including changes in sebum production and inflammation.
Multiorgan interaction studies: OOC systems can be designed to study interactions between skin and other organs (e.g., the endocrine system) that may influence acne development.
Conclusion
The study of acnegenesis models has significantly advanced our understanding of the pathophysiological mechanisms underlying acne. Various in vitro, in vivo, and ex vivo models, including human sebaceous glands, 3D skins models, and animal models like rodents and rabbits, have provided critical insights into the complex interplay between factors such as sebum production, hormonal regulation, microbial involvement, and immune response. However, each model has inherent limitations in mimicking the complexity of human acne, particularly in terms of long-term studies and accurately representing the unique interactions within human skin.
The emergence of advanced technologies, such as 3D bioprinting, organ-on-chip systems, and genetically modified animal models, holds promise for more precise and personalized acne research. These innovations, combined with traditional methods, will likely pave the way for more effective therapeutic approaches. Future studies should focus on refining these models to better capture the multifactorial nature of acne, improving predictive value, and enhancing translatability to clinical outcomes.
Ultimately, while progress has been made, there remains a need for further refinement in model development to fully unravel the intricacies of acnegenesis and to develop effective, targeted therapies. This comprehensive survey highlights the importance of integrating diverse acnegenesis models to create a robust framework for future acne research and treatment innovations.
The authors would like to acknowledge NETES Institute of Pharmaceutical Science, Santipur Mirza, for their support and assistance during the preparation of this manuscript.
- Leeming JP, Holland KT, Cuncliffe WJ. The microbial colonization of inflamed acne vulgaris lesions. Br J Dermatol. 1988;118(2):203-8. Available from: https://doi.org/10.1111/j.1365-2133.1988.tb01775.x
- Leyden JJ, McGinley KJ, Vowels B. Propionibacterium acnes colonization in acne and non-acne. Dermatology. 1998;196:55-8. Available from: https://doi.org/10.1159/000017868
- Dryden MS. Skin and soft tissue infection: microbiology and epidemiology. Int J Antimicrob Agents. 2009;34 Suppl 1:S2-7. Available from: https://doi.org/10.1016/s0924-8579(09)70541-2
- Sohail MR, Gray AL, Baddour LM, Tleyjeh IM, Virk A. Infective endocarditis due to Propionibacterium species. Clin Microbiol Infect. 2009;15:387-94. Available from: https://doi.org/10.1111/j.1469-0691.2009.02703.x
- Fleming A. On the etiology of acne vulgaris and its treatment by vaccines. Lancet. 1909;1:1035-8. Available from: https://doi.org/10.1016/S0140-6736(01)72096-X
- Thiboutot DM. Overview of acne and its treatment. Cutis. 2008;81:3-7. Available from: https://europepmc.org/article/med/18338651
- Melnik BC. Acne vulgaris: The metabolic syndrome of the pilosebaceous follicle. Clin Dermatol. 2018 Jan-Feb;36(1):29-40. Available from: https://doi.org/10.1016/j.clindermatol.2017.09.006
- Nakatsuji T, Kao MC, Fang JY, Zouboulis CC, Zhang L, Gallo RL, Huang CM. Antimicrobial property of lauric acid against Propionibacterium acnes: its therapeutic potential for inflammatory acne vulgaris. J Invest Dermatol. 2009;129(10):2480-8. Available from: https://doi.org/10.1038/jid.2009.93
- Kanwar IL, Haider T, Kumari A, Dubey S, Jain P, Soni V. Models for acne: a comprehensive study. Drug Discov Ther. 2018;12(6):329-40. Available from: https://www.academia.edu/90771847/Models_for_acne_A_comprehensive_study
- Mandrycky C, Wang Z, Kim K, Kim DH. 3D bioprinting for engineering complex tissues. Biotechnol Adv. 2016;34(4):422-34. Available from: https://iscrm.uw.edu/wp-content/uploads/2018/06/BiotechAdvJulAug16.pdf
- Bhatia SN, Ingber DE. Microfluidic organs-on-chips. Nat Biotechnol. 2014;32(8):760-72. Available from: https://doi.org/10.1038/nbt.2989
- Leyden JJ, McGinley KJ, Mills OH, Kligman AM. Age-related changes in the resident bacterial flora of the human face. J Invest Dermatol. 1975;65(4):379-81. Available from: https://doi.org/10.1111/1523-1747.ep12607630
- Unna PJ. Histopathology of the Diseases of Skin. Edinburgh. Clay. 1896.
- Sabouraud PR. Oily seborrhea and alopecia areata. Ann Inst Pasteur Microbiol. 1897;11:134-59.
- Kurokawa I, Danby FW, Ju Q, Wang X, Xiang LF, Xia L, et al. New developments in our understanding of acne pathogenesis and treatment. Exp Dermatol. 2009;18(10):821-32. Available from: https://doi.org/10.1111/j.1600-0625.2009.00890.x
- McGinley KJ, Webster GF, Leyden JJ. Regional variations of cutaneous propionibacteria. Appl Environ Microbiol. 1974;35:62-6. Available from: https://journals.asm.org/doi/pdf/10.1128/aem.35.1.62-66.1978
- McGinley KJ, Webster GF, Leyden JJ. Regional variations of density of cutaneous propionibacteria: correlation of P. acnes populations with sebaceous secretion. J Clin Microbiol. 1980;12:672-5. Available from: https://doi.org/10.1128/jcm.12.5.672-675.1980
- Toyoda M, Morohashi M. Pathogenesis of acne. Med Electron Microsc. 2001;34(1):29-40. Available from: https://link.springer.com/article/10.1007/s007950100002
- Xia LQ, Zouboulis C, Detmar M, Mayer-da-Silva A, Stadler R, Orfanos CE. Isolation of human sebaceous glands and cultivation of sebaceous gland-derived cells as an in vitro model. J Invest Dermatol. 1989;93(3):315-21. Available from: https://pubmed.ncbi.nlm.nih.gov/2671160/
- Zouboulis CC, Xia L, Akamatsu H, Seltmann H, Fritsch M, Hornemann S, et al. The human sebocyte culture model provides new insights into development and management of seborrhoea and acne. Dermatology. 1998;196:21-31. Available from: https://doi.org/10.1159/000017861
- Davis EC, Callender VD. A review of acne in ethnic skin: pathogenesis, clinical manifestations, and management strategies. J Clin Aesthet Dermatol. 2010;3(4):24-38. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC2921746/
- White GM. Recent findings in the epidemiologic evidence, classification, and subtypes of acne vulgaris. J Am Acad Dermatol. 1998;39(2 Pt 3):S34-7. Available from: https://doi.org/10.1016/s0190-9622(98)70442-6
- Yeung CK, Teo LH, Xiang LH, Chan HHL. A community-based epidemiological study of acne vulgaris in Hong Kong adolescents. Acta Derm Venereol. 2002;82:104-7. Available from: http://dx.doi.org/10.1080/00015550252948121
- Ghosh VK, Nagore DH, Kadbhane KP, Patil MJ. Different approaches of alternative medicines in acne vulgaris treatment. Orient Pharm Exp Med. 2011;11(1):1-9. Available from: https://link.springer.com/article/10.1007/s13596-011-0006-6
- Cordain L, Lindeberg S, Hurtado M, Hill K, Eaton SB, Brand-Miller J. Acne vulgaris: a disease of Western civilization. Arch Dermatol. 2002;138(12):1584-90. Available from: https://doi.org/10.1001/archderm.138.12.1584
- Mohan H. Textbook of Pathology. 4th ed. New Delhi: Jaypee Brothers. 2000;754-74.
- Zuo T, Chen H, Xiang S, Hong J, Cao S, Weng L, et al. Cryptotanshinone-Loaded Cerasomes Formulation: In Vitro Drug Release, in Vivo Pharmacokinetics, and in Vivo Efficacy for Topical Therapy of Acne. ACS Omega. 2016;1(6):1326-1335. Available from: https://doi.org/10.1021/acsomega.6b00232
- Chen T, Zhu Z, Du Q, Wang Z, Wu W, Xue Y, et al. A Skin Lipidomics Study Reveals the Therapeutic Effects of Tanshinones in a Rat Model of Acne. Front Pharmacol. 2021;12:675659. Available from: https://doi.org/10.3389/fphar.2021.675659
- Park SH, Lee JE, Lee SM, Lee J, Seo CS, Hwang GS, et al. An unbiased lipidomics approach identifies key lipid molecules as potential therapeutic targets of Dohongsamul-tang against non-alcoholic fatty liver diseases in a mouse model of obesity. J Ethnopharmacol. 2020;260:112999. Available from: https://doi.org/10.1016/j.jep.2020.112999
- Shen CY, Jiang JG, Li MQ, Zheng CY, Zhu W. Structural characterization and immunomodulatory activity of novel polysaccharides from Citrus aurantium Linn. variant amara. J Funct Foods. 2017;35:352-362. Available from: https://doi.org/10.1016/j.jff.2017.05.055
- Li D, Sun Y, Ren X, Zhou N, Li L, He G, et al. Dynamic evaluation of pathological changes in a mouse acne model by optical imaging technology. Exp Dermatol. 2023;32(9):1350-1360. Available from: https://doi.org/10.1111/exd.14826
- Fulton JE Jr, Pay SR, Fulton JE 3rd. Comedogenicity of current therapeutic products, cosmetics, and ingredients in the rabbit ear. J Am Acad Dermatol. 1984;10(1):96-105. Available from: https://doi.org/10.1016/s0190-9622(84)80050-x
- Artusi M, Nicoli S, Colombo P, Bettini R, Sacchi A, Santi P. Effect of chemical enhancers and iontophoresis on thiocolchicoside permeation across rabbit and human skin in vitro. J Pharm Sci. 2004;93(10):2431-2438. Available from: https://doi.org/10.1002/jps.20152
- Hikima T, Yamada K, Kimura T, Maibach HI, Tojo K. Comparison of skin distribution of hydrolytic activity for bioconversion of beta-estradiol 17-acetate between man and several animals in vitro. Eur J Pharm Biopharm. 2002;54(2):155-60. Available from: https://doi.org/10.1016/s0939-6411(02)00084-x
- Glasenhardt K, Erdei L, Bolla B, Tax G, Urbán E, Kemény L, et al. Development of an in vitro follicle model to study the interaction of keratinocytes, sebocytes, and Propionibacterium acnes. J Invest Dermatol. 2016;136(Suppl.):S223. Available from: http://dx.doi.org/10.1016/j.jid.2016.06.389
- Cibula D, Hill M, Vohradnikova O, Kuzel D, Fanta M, Zivny J. The role of androgens in determining acne severity in adult women. Br J Dermatol. 2000;143:399-404. Available from: https://doi.org/10.1007/s00403-012-1265-x
- Guy R, Ridden C, Kealey T. The improved organ maintenance of the human sebaceous gland: modeling in vitro the effects of epidermal growth factor, androgens, estrogens, 13-cis retinoic acid, and phenol red. J Invest Dermatol. 1996;106(3):454-60. Available from: https://doi.org/10.1111/1523-1747.ep12343608
- Raza K, Singh B, Singal P, Wadhwa S, Katare OP. Systematically optimized biocompatible isotretinoin-loaded solid lipid nanoparticles (SLNs) for topical treatment of acne. Colloids Surf B Biointerfaces. 2013;105:67-74. Available from: https://doi.org/10.1016/j.colsurfb.2012.12.043
- Xia LQ, Zouboulis C, Detmar M, Mayer-da-Silva A, Stadler R, Orfanos CE. Isolation of human sebaceous glands and cultivation of sebaceous gland-derived cells as an in vitro model. J Invest Dermatol. 1989;93(3):315-21. Available from: https://pubmed.ncbi.nlm.nih.gov/2671160/
- Toyoda M, Morohashi M. Pathogenesis of acne. Med Electron Microsc. 2001;34(1):29-40. Available from: https://doi.org/10.1007/s007950100002
- Huh D. A human gut-on-a-chip inhabited by microbial flora that experiences intestinal peristalsis. Sci Rep. 2010;5:15085.
- Grayson WL. A microfluidic skin model for testing drug permeation. Biotechnol Bioeng. 2015;112(12):2548-2559.
- Kim J. Development of a human skin-on-a-chip model using human dermal fibroblasts and keratinocytes. Biomaterials. 2016;106:67-75.
- Caffarel-Salvador E. Microfluidic skin-on-a-chip platform for drug testing. Lab Chip. 2016;16(12):2265-2273.
- Kligman AM, Leyden JJ, McGinley KJ. Bacteriology. J Invest Dermatol. 1976;67:160-168. Available from: https://doi.org/10.1111/1523-1747.ep12513007
- Nasiri M. Effect of isotretinoin on the skin of Wistar rats. J Dermatol Res. 2016.
- Shen C. Minocycline liposomes for acne treatment. J Pharm Sci. 2012.
- Nazzaro-Porro M. Azelaic acid as a topical treatment for acne. Br J Dermatol. 1993.
- Kong R. Berberine and acne treatment in rabbit models. Int J Anti-inflamm Drug. 2015.
- Mitchell T. Efficacy of salicylic acid in hamster sebaceous glands. Dermatol Res. 1995.
- Lee HS. Tea tree oil and its effect on acne in a murine model. Phytother Res. 2010.
- Elsaie ML. Green tea polyphenols and acne in mice models. Dermatol Ther. 2016.
- Kurokawa I. Clindamycin in rabbit models of acne. J Dermatol. 2011.
- Wei Y, Zhu X, Lin S, Yang W, Wang T, Nie X, et al. Zinc gluconate improves atopic dermatitis by modulating CXCL10 release of keratinocytes via PPARα activation. Biomed Pharmacother. 2024;177:117129. Available from: https://doi.org/10.1016/j.biopha.2024.117129
Article Alerts
Subscribe to our articles alerts and stay tuned.
 This work is licensed under a Creative Commons Attribution 4.0 International License.
This work is licensed under a Creative Commons Attribution 4.0 International License.


 Save to Mendeley
Save to Mendeley
